Diagnosing Back Pain And Prostate Cancer
A doctors first step in finding out the cause of back pain typically is to take an image, usually an X-ray or CT scan.
For men who have early stage or localized prostate cancer, that it would spread to the bone is very unusual, says Chris Filson, a doctor at the Atlanta Veterans Administration Medical Center. However, if a patient has more advanced prostate cancer, we have to do additional tests to ensure theres no involvement of the cancer in the bone.
A doctor who suspects or already has diagnosed prostate cancer will look for characteristic changes in the bone. The X-ray or CT scan also can indicate how much of your spine is affected and where.
In addition, an MRI can detect problems that an X-ray or CT scan cant.
Chiropractors are often the ones who first spot or suggest the presence of prostate cancer. Joint pain, especially back pain, often sends people to chiropractic care when they dont have any other symptoms of prostate cancer.
Whether youre seeing a chiropractor or medical doctor, be sure to provide your complete medical history. This can help your doctor diagnose your back pain. Its especially important to mention any personal or family history of cancer.
Is Another Treatment Option Better For Preservation Of Erectile Function
The growing interest in pelvic radiation, including brachytherapy, as an alternative to surgery can be attributed in part to the supposition that surgery carries a higher risk of erectile dysfunction. Clearly, surgery is associated with an immediate, precipitous loss of erectile function that does not occur when radiation therapy is performed, although with surgery recovery is possible in many with appropriately extended follow-up. Radiation therapy, by contrast, often results in a steady decline in erectile function to a hardly trivial degree over time.
Introduction To Nerve Regeneration
Three sets of nerves are important when a man has sex:
Because of their location, sandwiched between the prostate and the rectum, the second set of nerves can be affected during radical prostatectomy. The other two sets of nerves cannot be affected. Regarding climax after surgery, roughly 80% of men describe climax as being equally satisfying after surgery as before, 10% say that it is better and 10% say that it is less intense.
Recommended Reading: Can An Enlarged Prostate Cause Constipation
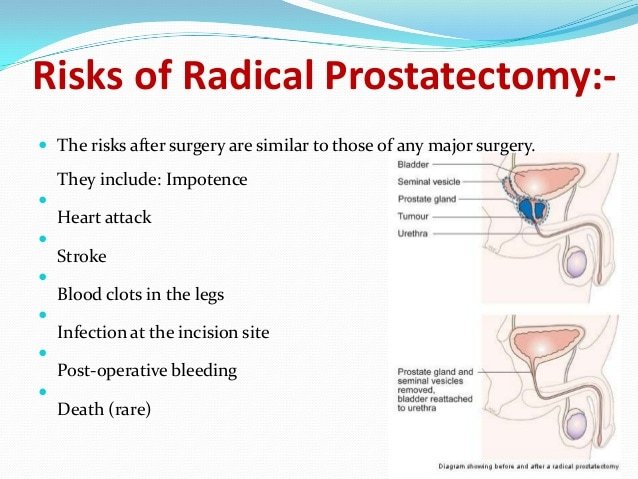
Side Effects Of Prostate Surgery
The major possible side effects of radical prostatectomy are urinary incontinence and erectile dysfunction . These side effects can also occur with other forms of prostate cancer treatment.
Urinary incontinence: You may not be able to control your urine or you may have leakage or dribbling. Being incontinent can affect you not only physically but emotionally and socially as well. These are the major types of incontinence:
- Men with stress incontinence might leak urine when they cough, laugh, sneeze, or exercise. Stress incontinence is the most common type after prostate surgery. It’s usually caused by problems with the valve that keeps urine in the bladder . Prostate cancer treatments can damage this valve or the nerves that keep the valve working.
- Men with overflow incontinence have trouble emptying their bladder. They take a long time to urinate and have a dribbling stream with little force. Overflow incontinence is usually caused by blockage or narrowing of the bladder outlet by scar tissue.
- Men with urge incontinencehave a sudden need to urinate. This happens when the bladder becomes too sensitive to stretching as it fills with urine.
- Rarely after surgery, men lose all ability to control their urine. This is called continuous incontinence.
After surgery for prostate cancer, normal bladder control usually returns within several weeks or months. This recovery usually occurs slowly over time.
There are several options for treating erectile dysfunction:
Side Effects From Radiation
Urinary symptoms from radiation treatment for prostate cancer are different from those caused by prostate surgery. “It’s more like a urinary tract infection-increased urgency and frequency, and men may some have bleeding or pain when they urinate,” Calvaresi said. These problems often go away once treatment is complete.
Radiation also may cause bowel changes, such as constipation, loose stools or both. These can be managed by over-the-counter medication. Men may also see some blood in their stool during treatment-if so, let your health care provider know about this.
Men undergoing radiation are likely to have ED, but not immediately. “It slowly sets in after radiation treatment,” Calvaresi said. Treatments for radiation-related ED are the same as ED caused by prostate cancer surgery.
Don’t Miss: Does Cialis Shrink The Prostate
Your Emotions And Sex
Your prostate cancer and its treatment wonât just affect your body. Theyâll also have a serious impact on your emotions. Stress and anxiety can trigger your body to make adrenaline, which gets in the way of having sex. The more you worry, the worse the struggle. If youâre in a relationship, your partner will be going through many of the same feelings.
One of the most important things you can do is to talk to your partner. Have an honest conversation about your fears and expectations when it comes to sex. Don’t assume they know how you feel. Being open with each other will help you both feel supported and help you work together to make any adjustments that you may need to stay intimate.
Talking with a mental health professional — either one-on-one or with your partner — can be a powerful way to help manage your emotions. A therapist can also prescribe medications that may ease stress and anxiety. A professional sex therapist can help you and your partner find ways to improve your sex life. It may also be helpful to join a support group where you can talk with others who share your experience.
Prostate Cancer Foundation: “Erectile Dysfunction.”
UCLA Urology: “Prostate Cancer: Dealing with Erectile Dysfunction.”
Albaugh, J. Reclaiming Sex & Intimacy After Prostate Cancer: A Guide for Men and Their Partners. Anthony J. Jannetti, Inc., 2012.
Harvard Prostate Knowledge: “Achieving orgasm after radical prostatectomy.”
Remission And The Chance Of Recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having no evidence of disease or NED.
A remission can be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. Although there are treatments to help prevent a recurrence, such as hormonal therapy and radiation therapy, it is important to talk with your doctor about the possibility of the cancer returning. There are tools your doctor can use, called nomograms, to estimate someone’s risk of recurrence. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence.
In general, following surgery or radiation therapy, the PSA level in the blood usually drops. If the PSA level starts to rise again, it may be a sign that the cancer has come back. If the cancer returns after the original treatment, it is called recurrent cancer.
When this occurs, a new cycle of testing will begin again to learn as much as possible about the recurrence, including where the recurrence is located. The cancer may come back in the prostate , in the tissues or lymph nodes near the prostate , or in another part of the body, such as the bones, lungs, or liver . Sometimes the doctor cannot find a tumor even though the PSA level has increased. This is known as a PSA-only or biochemical recurrence.
Don’t Miss: Does Prostatitis Go Away Without Treatment
What Happens During My Operation
A general anaesthetic will be used you will be asleep throughout the procedure. During surgery, you will be given antibiotics by injection.
Robotic-Assisted Laparoscopic Prostatectomy
Robotic surgery is performed via keyhole incisions and uses sophisticated mini-instruments which are under the control of the surgeon. The robot mimics and assists the surgeons movements; it does not do the operation. The technique is now widely used because of its high degree of surgical accuracy, and because your recovery is faster than it is for open surgery.
Six small incisions are made into the abdomen through which the robotic instruments are inserted. The robot is placed beside you in the operating theatre. The robot has four arms – three for instruments and one for a high magnification 3-D camera to allow the surgeon to see inside your abdomen. The robotic instruments are small approximately 7mm in width. The surgeon sits in the same rooms but away from the patient and with the robotic technology is able to carry out more controlled and precise movements in a small space within the body.
The muscle fibres and nerves that control continence are preserved.
The skin is closed with absorbable sutures which are located under the skin and are not visible and the outside is sealed with skin glue.
Blood loss is usually less than 200mL and the risk of a blood transfusion <2%
Open Prostatectomy
Blood loss is usually around 500mL. The risk of a blood transfusion in my hands is <2%.
How To Return To An Active Sex Life After Prostate Cancer Treatment
No matter the cancer, treatments often cause side effects that affect patients quality of life. But with prostate cancer, the potential side effects can be particularly concerning to men who are trying to decide which approach is right for them. Surgery, radiation therapy and other treatments may impact a patients sex life, causing challenges like low sex drive, loss of penis length, dry orgasm or low sperm counts. Despite the angst these issues may cause, experts say most of these side effects can be managed and many men have a good chance of returning to a full sex life after prostate cancer treatment.
Unfortunately, sexual dysfunction is a possibility for nearly all treatment options for prostate cancer, including surgery, says Scott Shelfo, MD, FACS, Medical Director of Urology at our hospital near Atlanta.;The degree of dysfunction depends on many factors, including the patients overall health, co-existing medical problems, as well as the patients level of sexual function and ability before treatment.
Read Also: Does An Enlarged Prostate Affect A Man Sexually
If Treatment Does Not Work
Recovery from cancer is not always possible. If the cancer cannot be cured or controlled, the disease may be called advanced or terminal.
This diagnosis is stressful, and for many people, advanced cancer may be difficult to discuss. However, it is important to have open and honest conversations with your health care team to express your feelings, preferences, and concerns. The health care team has special skills, experience, and knowledge to support patients and their families and is there to help. Making sure a person is physically comfortable, free from pain, and emotionally supported is extremely important.
People who have advanced cancer and who are expected to live less than 6 months may want to consider hospice care. Hospice care is designed to provide the best possible quality of life for people who are near the end of life. You and your family are encouraged to talk with the health care team about hospice care options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment, including a hospital bed, can make staying at home a workable option for many families. Learn more about advanced cancer care planning.
After the death of a loved one, many people need support to help them cope with the loss. Learn more about grief and loss.
Does Penis Length Recover After Prostate Removal
By Andrew M. Seaman, Reuters Health
5 Min Read
– After prostate removal for cancer, men sometimes complain to their doctors that their penis shrank, but a new study from Japan suggests they should not lose hope.
Following men for up to two years after surgery, researchers found the patients penises were shortest a few days after their procedures. Penis lengths generally returned to normal after one year, however.
The studys lead author said the research was started after encountering a few patients complaining of penis shortening after prostate removal, which is known medically as a radical prostatectomy.
Past reports mentioned shortened penises after prostate removal, but the results were a bit different, said Dr. Yoshifumi Kadono, of Kanazawa University Graduate School of Medicine Science.
Therefore, we started our study to obtain our data, he told Reuters Health.
For the new study, the researchers measured the penis lengths of 102 men before having their prostates removed and then at 10 days after surgery and again one, three, six, nine, 12, 18 and 24 months later.
The mens stretched penis lengths were shortest 10 days after surgery, when measurements were an average of about 1.99 centimeters shorter than before prostate removal.
The researchers wanted to know what caused the shortening and if any particular variable, such as the size of a mans prostate gland, would predict which men would experience this effect.
Don’t Miss: Can Bph Cause Constipation
Intracavernosal Injection And Intraurethral Therapy
ICI and intraurethral therapy use alprostadils vasodilation effects to improve EF. Alprostadil delivers prostaglandin E1 which increases the levels of 3′,5′-cyclic adenosine monophosphate within the erectile tissue and result in the efflux of intracellular calcium ions and cavernosal smooth muscle relaxation. Its intraurethral form generally does not cause systemic side-effects, but locally it can elicit urethral burning and penile pain . Trials investigating non-oral and non-pharmacological therapies are summarized in Table 2.
Table 2
McCullough et al. presented the first randomized, prospective trial to study the effect of intraurethral alprostadil with Medicated Urethral System for Erection . Two hundred and twelve men were randomized into taking nightly IUA or nightly sildenafil for 9 months. IUA was titrated from 125 to 250 µg after 1 month of treatment for better toleration of side effects. At study end, there was no statistically significant difference in the IIEF-EF score or successful intercourse rates. They did note a significant difference between groups in erections, assessed by the global assessment question, at 6 months in favor of IUA . Although compliance rates were 98% and 79% for sildenafil and IUA, respectively, dropout rates approximated 30% for the IUA group secondary to pain experienced after the increase in IUA dosage.
What Should I Expect When I Get Home
When you are discharged from the ward you will need some baggy trousers or track pants as you may find that your abdomen is uncomfortable and the catheter is easier to manage if your clothing is loose.
There will be some blood, urine and mucus which passes ALONGSIDE or through the catheter and is particularly noticeable after passing a bowel motion this is normal. You should wash the area with soap and water to remove this discharge to reduce any irritation. Keeping a high oral fluid intake reduces the risk of catheter blockage.
You may notice some swelling and bruising around the wounds, the penis and the scrotum which takes several weeks to resolve. You may also notice small firm lumps below the wound these are normal and are simply the knots in the suture material used to close the wound. The suture slowly dissolves and will disappear within 3 months. Most men feel quite tired after surgery and this takes several weeks to resolve.
Following surgery, you will be given a prescription for regular pain medication as well as some laxative medication to keep your bowels regular and thus avoid any straining.
Light walking is encouraged straight after the surgery. After four weeks you may resume heavy lifting.
Showering, bathing and getting the wounds wet is fine the skin has been sealed with glue.
Driving is safe once you are comfortable to do so and feel able to make an emergency stop. This would normally be around 3 weeks following surgery.
Read Also: How To Massage A Man’s Prostate
Later Reports On Nerve Grafts
Anastasiadis AG, Benson MC, Rosenwasser MP, et al. Cavernous Nerve Graft Reconstruction During Radical Prostatectomy or Radical Cystectomy: Safe and Technically Feasible. Prostate Cancer and Prostatic Diseases 2003;6:5660. PMID: 12664067.
Hanson GR, Borden LS Jr., Backous DD, et al. Erectile Function Following Unilateral Cavernosal Nerve Replacement. Canadian Journal of Urology 2008;15:399093. PMID: 18405447.
Joffe R, Klotz LH. Results of Unilateral Genitofemoral Nerve Grafts With Contralateral Nerve Sparing During Radical Prostatectomy. Urology 2007;69:116164. PMID: 17572207.
Namiki S, Saito S, Nakagawa H, et al. Impact of Unilateral Interposition Sural Nerve Graft on Recovery of Potency and Continence Following Radical Prostatectomy: 3-Year Longitudinal Study. Journal of Urology 2007;178:21216. PMID: 17499797.
Nelson BA, Chang SS, Cookson MS, Smith JA Jr. Morbidity and Efficacy of Genitofemoral Nerve Grafts With Radical Retropubic Prostatectomy. Urology 2006;67:78992. PMID: 16584763.
Sim HG, Kliot M, Lange PH, et al. Two-Year Outcome of Unilateral Sural Nerve Interposition Graft After Radical Prostatectomy. Urology 2006;68:129094. PMID: 17141842.
Singh H, Karakiewicz P, Shariat SF, et al. Impact of Unilateral Interposition Sural Nerve Grafting on Recovery of Urinary Function After Radical Prostatectomy. Urology 2004;63:112227. PMID: 15183964.
What Typically Increases The Risk Of Complications From Prostate Cancer Surgery
Complication risks can be increased if prior surgery for unrelated reasons was done in the area or if we have to do extensive surgery to remove the cancer. But complication rates also go up dramatically when we do surgery on patients who have failed other prostate cancer treatments, such as radiation therapy.
Radiation is a very effective treatment for prostate cancer, but it doesnt work for everyone. In these patients, we often believe the cancer has recurred or persisted in the prostate without spreading, so removing the prostate following failed radiation treatment a procedure called salvage prostatectomy is potentially curative.
Salvage prostatectomy is more technically challenging than radical prostatectomy. Patients who have already had radiation therapy often have scarring in and around the prostate, which can make tissue in the area very difficult to separate while performing the operation. As a result, patients undergoing salvage prostatectomy have a much higher risk of urinary incontinence, and a higher rate of developing more scar tissue, strictures ;which is a narrowing of the urethra that blocks urine flow or injury to adjacent structures like the rectum.
Read Also: Does An Enlarged Prostate Affect A Man Sexually
