Sexual Dysfunction And Gynecomastia
Several studies have shown that treatment for clinically localized prostate cancer involving either radical prostatectomy, brachytherapy, or external beam radiotherapy can result in long-term erectile dysfunction. Patients receiving neoadjuvant ADT with EBRT were found to have decreased frequency of erection, decreased overall sexual function, and an increase in frequency of hot flushes. In addition, loss of libido is a major consequence of ADT. The degree of erectile dysfunction for patients on ADT is impacted by pretreatment sexual function, as well as by changes in libido in patients previously able to attain an erection, phosphodiesterase 5 inhibitors, intracavernosal injection therapy, vacuum-assisted devices, or other topical agents may be used. Given the complex interplay between physiology, psychology, stress, and emotion involved in sexual function, a referral to a psychology or counseling service with a focus on sexual health is recommended for interested patients and their partners.
Locally Advanced Prostate Cancer
In the 1980s, patients with locally advanced prostate cancer were treated definitively with radiation therapy. However, the risk of locoregional failures after radiation therapy was known to increase with higher initial disease burden . With the success of ADT in the metastatic setting, the Radiation Therapy Oncology Group initiated a series of trials to evaluate the potential benefits of cytoreductive ADT delivered in combination with definitive radiation therapy in an effort to improve disease control.
In 1983, RTOG launched a phase II clinical trial, RTOG 83-07, to evaluate the clinical effectiveness and potential toxicity of diethylstilbestrol , a synthetic nonsteroidal estrogen, versus megestrol, a steroidal progestin, in prostate cancer patients with organ-confined disease or extension beyond the prostate . DES proved to more toxic than megestrol with comparable rates of local failure .
The authors of RTOG 85-19 noted that the mechanism of interaction between radiation therapy and androgen deprivation in carcinoma of the prostate remain largely unknown. They suggested that in addition to reducing tumor volume, when offered concurrently with radiation therapy, ADT may interact with radiation on a cellular level. .
Together, RTOG 92-02 and EORTC 22863 demonstrated a clinically meaningful benefit of long-term ADT delivered concurrently with definitive radiation therapy for patients with locally advanced, high-risk disease, which remains the standard of care .
Drugs In Development Targeting The Androgen Pathway
Other ADT drugs include darolutamide and relugolix that are not yet approved. Darolutamide is an oral, nonsteroidal antiandrogen with a similar mode of action to enzalutamide and apalutamide. In a 12-week phase 2 study, darolutamide demonstrated a PSA response rate of 29% in the low, 33% in the mid, and 33% in the highest dose group .
Relugolix is an oral GnRH antagonist in phase 3 development. In healthy males the drug was readily absorbed and reduced mean serum T levels within 6h of dosing however, a food effect reduced exposure by 50%. T recovered rapidly following cessation of treatment .
Patients may prefer oral dosing over injections due to the convenience of not requiring a clinic visit for injections and the avoidance of injection-site AEs however, there may be disadvantages. Compliance with oral dosing is rarely 100%, especially for long-term treatments where dosing may be required for months or years and particularly where the underlying illness is asymptomatic. Missed doses may compromise efficacy, which may be critical when the illness is serious or life threatening e.g., use of statins or antihypertensives in patients with cardiovascular disease and dosing of cancer treatments . With ADT, this issue can be avoided and 100% compliance achieved if the therapy is given on schedule via long-acting injection. Due to the high daily doses of drug required for the androgen pathway inhibitors, depot injections may not be feasible.
Read Also: When Should Men Get A Prostate Exam
Early Versus Delayed Treatment
For men who need hormone therapy, such as men whose PSA levels are rising after surgery or radiation or men with advanced prostate cancer who dont yet have symptoms, its not always clear when it is best to start hormone treatment. Some doctors think that hormone therapy works better if its started as soon as possible, even if a man feels well and is not having any symptoms. Some studies have shown that hormone treatment may slow the disease down and perhaps even help men live longer.
But not all doctors agree with this approach. Some are waiting for more evidence of benefit. They feel that because of the side effects of hormone therapy and the chance that the cancer could become resistant to therapy sooner, treatment shouldnt be started until a man has symptoms from the cancer. This issue is being studied.
Systemic Therapy For High
The utility of combining ADT with radiotherapy has often been questioned, especially in the setting of dose escalation. In fact, NCCN guidelines for both high- and very high risk prostate cancer include ADT as an option, rather than necessity, when EBRT is combined with low dose rate brachytherapy boost however, a recent network meta-analysis suggests that EBRT and ADT may result in superior overall survival compared to patients treated with EBRT and brachytherapy boost . In the DART01/05 GICOR study, where about 50% patients belonged to the high-risk category, 28 months of long-term ADT combined with 78 Gy of external beam radiotherapy was associated with significantly superior overall and metastasis-free survival compared to 4 months of ADT with same dose of EBRT . In the TROG 03.04 RADAR trial, where approximately two-thirds of patients belonged to the high-risk group, it was found that 18 months of ADT reduced distant progression compared to 6 months of ADT, regardless of radiotherapy dose . Similarly, in the EORTC 22991 trial, 6 months of adjuvant ADT significantly improved biochemical disease-free survival and clinical progression-free survival across all radiation dose levels . All these findings, taken together, confirm that dose-escalation and ADT synergize with each other by enhancing local and distant control, respectively.
Recommended Reading: What To Say To Someone With Prostate Cancer
Cellular Mechanism Of Action
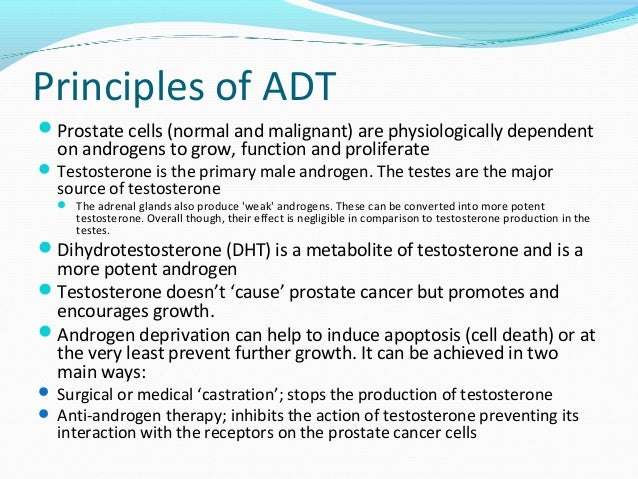
While ADT was being developed clinically for use in patients with prostate cancer, others were investigating the mechanism by which suppression of androgens improves disease control. There was conjecture about the clinical benefit of ADT being a result of cytoreduction or debulking of disease prior to radiation therapy, while others surmised a synergy between ADT and radiation therapy at the cellular level.
In men, the majority of circulating testosterone is produced by leydig cells in the testes following stimulatory signals produced by the pituitary, LH and FSH. The remainder of testosterone is produced by the adrenal gland, derived from circulating steroid hormone precursors . Once produced, testosterone is transported protein-bound to the target cell where it is metabolized intracellularly by 5-reductase to the super-active metabolite, dihydrotestosterone . DHT binds its cognate receptor, the AR, which subsequently dimerizes and is translocates into the nucleus where it conducts its DNA-directed functions, including transcriptional regulation of target genes .
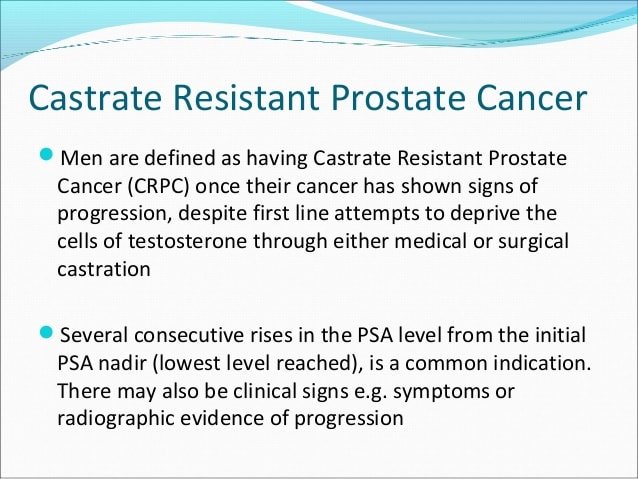
The critical importance of AR-signaling for prostate cancer growth is further highlighted in the context of castrate resistant prostate cancer, prostate cancer that grows despite androgen levels being suppressed to castrate levels. In these patients, exogenous selection pressure stimulates resistance to ADT through multiple pathways.
Sequence Of Adt With Radiation Is Crucial For Prostate Cancer Treatment
The sequence in which hormonal therapy is given to men with localized prostate cancer should be considered as it can significantly affect outcomes, according to pooled data from 2 phase 3 clinical trials.
A team of researchers led by Daniel Spratt, MD, a professor of radiation oncology at the University of Michigan, conducted a systematic literature search using MEDLINE, Embase, trial registries, and major urology and oncology conference proceedings to retrieve studies that evaluated the optimal sequencing of definitive radiation therapy with androgen deprivation therapy in men with localized prostate cancer.
Patient data were collected after their search was narrowed to 2 studiesthe NRG Oncologys Radiation Therapy Oncology Group 9413 trial and the randomized Ottawa 0101 trial. In the latter trial, patients were randomly assigned to neoadjuvant or concurrent vs concurrent or adjuvant short-term ADT. RTOG 9413 included a random assignment of neoadjuvant or concurrent vs adjuvant short-term ADT.
The primary endpoint was progression-free survival , and secondary endpoints included metastasis-free survival and overall survival .
Data from more than 1000 patients were examined. The median age was 70 years, 58.1% had a Gleason score of 7 and 16.9% had a Gleason score of 8 to 10. Nearly 20% of patients had clinical T3 and T4 disease, and the median prostate-specific antigen was 14.1 ng/mL.
Also Check: How To Regain Bladder Control After Prostate Surgery
Adt And Neuroendocrine Differentiation
The emergence of neuroendocrine differentiation following prolonged ADT is a well-recognized phenomenon in prostate cancer. The rapid autopsy study of Shah et al. found NE differentiation in 10% of cases with castrate-resistant disease. It manifests clinically as an expanding tumor burden, often with a stable serum PSA and castrate levels of testosterone, and metastases to sites not commonly seen in usual acinar-type prostate cancer. NE differentiation can also be an incidental finding in palliative transurethral resection of prostate specimens in patients treated with primary ADT . Prostate cancers showing NE differentiation following ADT are typically AR-negative on immunohistochemical staining and are not given Gleason scores.
Guidelines For Assessing Cognitive Function In Prostate Cancer Patients
| – Environmental memory task encoding and recognition judgment of line orientation- Puget sound route learning test- Vandenberg and Kuse mental rotation test- Visuo-motor integration test block design |
Data from Kulkarni & Moningi and McGinty et al. .D-KEFS, Delis-Kaplan executive function system WAIS-R, Wechsler adult intelligence scale-revised WAIS-III, Wechsler adult intelligence scale-third edition WMS-R, Wechsler memory scales-re-vised edition WMS-III, Wechsler memory scales-third edition.
You May Like: Is Stage 3 Prostate Cancer Serious
Importance Of New Imaging Modalities And Molecular Imaging
Conventional clinical staging with digital rectal exam, PSA, random and systematic biopsies, with or without CT, pelvic lymphadenectomy, and bone scans have modest accuracy and the ability to define both location and burden of disease . In fact, it is estimated that conventional staging underestimates the location and burden of disease by 2030% , which can lead to undertreatment and subsequent relapse of disease. In the high-risk setting, the window for cure is correlated to the accurate detection of the extent of clinically significant prostate cancer .
Disease identification has been improved with the use of mpMRI and positron emission tomography . MpMRI, with T2-weighted images, diffusion-weighted imaging , and dynamic contrast-enhanced images, are state-of-the-art imaging modalities to assess the local extent of prostate cancer . The use of mpMRI increased the rate of detection of clinically significant cancer by 30% compared to the standard 12-core biopsy . Specifically in the context of high-risk disease, T2W images have close to 100% sensitivity and specificity for identifying seminal vesicle invasion, and sensitivity as high as 7590% for identifying extraprostatic extension .
These studies highlight the role of new imaging modalities and their potential role to guide personalized treatment for patients.
Lowering Adrenal Gland Androgen Levels
Because LHRH agonists and antagonists only lower testosterone production levels in the testicles, other treatments may be needed to lower androgens made by the adrenal glands or the prostate cancer itself.
Medications that lower adrenal gland androgen levels include:
- Zytiga® : Taken orally each day, this treatment is often used when cancer has spread to the bones or if the patient is high-risk or has castrate-resistant prostate cancer, meaning its still growing despite low testosterone levels.
- Nizoral® : This treatment is also taken orally and works similarly to abiraterone. Its also used in men with advanced prostate cancer whose cancer has spread.
You May Like: Does Krill Oil Cause Prostate Cancer
Chemotherapy And Immune Therapy
Contemporary and emerging options for androgen-independent, systemically advanced prostate cancer include chemotherapy and immune-based approaches. These approaches have historically been used as palliative measures. Most pathologists would not encounter diagnostic specimens from these patients aside from autopsy, palliative TURP procedures, or biopsies performed as part of clinical trials. As such, there are few published descriptions of treatment-induced changes in the morphology of prostate cancer in this setting. A complicating issue with respect to assessing treatment-induced changes specific to these agents in androgen-independent disease, is the fact that most if not all of these patients will have been treated with ADT and/or RT and possibly salvage ablative therapy. Nonetheless, as new clinical trials for hormone-sensitive and -resistant prostate cancer appear, pathologists will be required to review biopsies to document treatment-related changes that could signal hope to patients with an otherwise dismal prognosis.
Andropause And The Treatment Nobody Talks About
Who should not get ADT? Anybody else with prostate cancer. If you just have a rising PSA after radiation therapy or radical prostatectomy, that is not a good enough reason for a doctor to put you on ADT. If your doctor wants to put you on ADT to shrink your prostate before brachytherapy, thats not a good enough reason.
ADT has never been shown to extend life if its given too soon.
Why not just give it? At least its doing something, rather than sitting around waiting for the cancer to spread. Well, that sounds good. Please refer to the previous paragraph, and read the last sentence again. Now, if you have a rising PSA, there are other things you can do that may help a lot. These include:
- Salvage surgery or radiation, if your doctor thinks the cancer is still confined to the prostate bed, the area around the prostate.
- Immunotherapy a vaccine such as Provenge, designed to boost your bodys ability to fight off the cancer.
- Early chemotherapy.
- A clinical trial testing a promising new drug.
Dont get us wrong were not hating on ADT. If you need it, you need it. But its not just like taking a vitamin supplement or getting a flu shot. There are serious side effects with long-term ADT things that testosterone normally helps protect you from including thinning of bones, loss of muscle mass, weight gain, loss of libido, hot flashes, mood changes, depression and, our main subject here, the risk of cognitive impairment.
All of this is magnified with ADT.
Also Check: Can A Man Get An Erection After Prostate Surgery
How Will I Know That My Hormone Therapy Is Working
Doctors cannot predict how long hormone therapy will be effective in suppressing the growth of any individual mans prostate cancer. Therefore, men who take hormone therapy for more than a few months are regularly tested to determine the level of PSA in their blood. An increase in PSA level may indicate that a mans cancer has started growing again. A PSA level that continues to increase while hormone therapy is successfully keeping androgen levels extremely low is an indicator that a mans prostate cancer has become resistant to the hormone therapy that is currently being used.
Adverse Events Of Lhrh Agonists
The adverse events associated with LHRH agonists can be categorized as immediate, acute, and chronic. The optimal use of ADT requires an effort to prevent or treat these adverse events.
One of the limitations of LHRH agonists is the initial flare phenomenon, which is attributed to a surge of serum testosterone levels due to the initial stimulation of LHRH receptors.13 The flare phenomenon may be life threatening if an LHRH agonist is administered to men with high-volume metastatic disease. The clinical consequence of the flare is prevented by pretreatment with an antiandrogen, which inhibits the stimulatory effect of the testosterone surge at the level of the androgen receptor.14
Men with advanced prostate cancer are also predisposed to developing anemia due to hematuria from locally advanced prostate cancer and to bone marrow infiltration by metastatic disease. Testosterone increases production of erythrogenesis-stimulating proteins.22 Therefore, LHRH agonists may cause or exacerbate anemia by indirectly inhibiting erythrogenesis.
Progressive muscle loss has been associated with declining testosterone levels in men.15 Men receiving LHRH agonists for prostate cancer demonstrate significant increases in muscle fatigue.23 Resistance exercises may limit the consequences of LHRH agonists on muscle function.
Don’t Miss: How Long Does Prostate Laser Surgery Take
Considerations For Initiating Adt After Biochemical Recurrence In Prostate Cancer
Raoul S. Concepcion, MD, FACS:When you do have a biochemical recurrence, youve defined what that looks like for you regarding surgery and radiation. I think Judd has brought up some very good points relative to looking at the initial Gleason at the time of therapy, especially in the patients with radical prostatectomy . I think thedata spelled that out at . What are the factors that are going to say, like you said, just because you have a biochemical recurrence and a rise in the PSA doesnt necessarily mean its cancer cells it could be benign cells. What are the parameters? What are some of the things that are going to push you to say, I better initiate ADT in this patient?
Brian Helfand, MD, PhD: Or some form of therapy. I think that is a lot of the art form. I think its not a simple straightforward that everyone who has a biochemical recurrence needs treatment. If you look at the data, not everyone who has a biochemical recurrence will ultimately go on to succumb from prostate cancer or develop obvious metastasis. I think that the timing of the recurrence is imperative. Notably, someone who has a PSA recurrence 10 or 15 years later is different than the guy who has a recurrence almost immediately, or within a few months following treatment.
Transcript edited for clarity.
Weighing Pros And Cons Of Adt
ADT reduces levels of male hormones in the body, called androgens, to stop them from helping prostate cancer cells grow. It can help some men with high-risk localized or advanced prostate cancer live longer.
But ADT can often cause negative side effects that include reduced sexual desire, impotence, hot flashes, osteoporosis, loss of muscle mass, and depression. The study authors say the risk of dementia is one more possible negative side effect that should be considered when weighing the benefits and risks of ADT, especially for men who have a longer life expectancy because it takes time to develop dementia.
Read Also: Do Over The Counter Prostate Meds Work
