How Should I Prepare
Your MRI exam may use anendorectal coil, a thin wire covered with a latex balloon. The doctor places the coil a short distance into the rectum. The rectum is located immediately behind and up against the prostate. Placing the coil into the rectum so close to the prostate helps generate more detailed images. It also enables yourradiologist to perform magnetic resonance spectroscopy. MR spectroscopy can provide additional information on the chemical makeup of cells in the prostate. Additionally, prostate MRI may examine water molecule motion and blood flow within the prostate to help differentiate between diseased and normal prostate tissue.
Your doctor will typically use an endorectal coil with low-field MRI magnets if you have a metal orthopedic implant. Metal implants may interfere with imaging when using a high-field magnet MRI. The doctor will typically not use an endorectal coil with high-field MRI units.
You will need to change into a hospital gown. This is to prevent artifacts appearing on the final images and to comply with safety regulations related to the strong magnetic field.
Guidelines about eating and drinking before an MRI vary between specific exams and facilities. Take food and medications as usual unless your doctor tells you otherwise.
If you have claustrophobia or anxiety, ask your doctor to prescribe a mild sedative prior to the date of your exam.
- some cochlear implants
Donât Miss: How Long Can You Live With Gleason 6 Prostate Cancer
Diagnosis Of Extracapsular Extension
Imaging findings suggesting extraprostatic extension:
- Soft tissue tumor growing over the capsule
- Capsular bulging or irregularity
- > 1cm and certainly as indicated above
- 2cm of abutment = 82% likelihood
- Filling in of the rectoprostatic angle, posterolaterally on T1WI
- Asymmetry or invasion of the neurovascular bundles
- Capsular contact for predicting extracapsular extension
- > 2 cm: an accuracy of 82%
- < 1 cm: the chance of extracapsular extension was 5%
MRI Findings in T3 Disease with Capsular Signs of InvolvementRadiology 1997 202: 697-702 and 2005 237: 541-549Abbreviations: RP = Rectoprostatic angle NVB = Neurovascular Bundle
T-stage of TNM classification for prostate cancer
Imaging Tests For Prostate Cancer
Imaging tests use x-rays, magnetic fields, sound waves, or radioactive substances to create pictures of the inside of your body. One or more imaging tests might be used:
- To look for cancer in the prostate
- To help the doctor see the prostate during certain procedures
- To look for spread of prostate cancer to other parts of the body
Which tests you might need will depend on the situation. For example, a prostate biopsy is typically done with transrectal ultrasound and/or MRI to help guide the biopsy. If you are found to have prostate cancer, you might need imaging tests of other parts of your body to look for possible cancer spread.
The imaging tests used most often to look for prostate cancer spread include:
You May Like: Why Is My Prostate Hurting
Biopsy During Surgery To Treat Prostate Cancer
If there is more than a very small chance that the cancer might have spread , the surgeon may remove lymph nodes in the pelvis during the same operation as the removal of the prostate, which is known as a radical prostatectomy .
The lymph nodes and the prostate are then sent to the lab to be looked at. The lab results are usually available several days after surgery.
What Are Grade Groups
Grade Groups are a new way to grade prostate cancer to address some of the issues with the Gleason grading system.
As noted above, currently in practice the lowest Gleason score that is given is a 6, despite the Gleason grades ranging in theory from 2 to 10. This understandably leads some patients to think that their cancer on biopsy is in the middle of the grade scale. This can compound their worry about their diagnosis and make them more likely to feel that they need to be treated right away.
Another problem with the Gleason grading system is that the Gleason scores are often divided into only 3 groups . This is not accurate, since Gleason score 7 is made up of two grades , with the latter having a much worse prognosis. Similarly, Gleason scores of 9 or 10 have a worse prognosis than Gleason score 8.
To account for these differences, the Grade Groups range from 1 to 5 :
- Grade Group 1 = Gleason 6
- Grade Group 2 = Gleason 3+4=7
- Grade Group 3 = Gleason 4+3=7
- Grade Group 4 = Gleason 8
- Grade Group 5 = Gleason 9-10
Although eventually the Grade Group system may replace the Gleason system, the two systems are currently reported side-by-side.
Read Also: How To Properly Massage Prostate
What Gets Stored In A Cookie
This site stores nothing other than an automatically generated session ID in the cookie no other information is captured.
In general, only the information that you provide, or the choices you make while visiting a web site, can be stored in a cookie. For example, the site cannot determine your email name unless you choose to type it. Allowing a website to create a cookie does not give that or any other site access to the rest of your computer, and only the site that created the cookie can read it.
What Do My Test Results Mean
Your doctor will look at your test results to find out if the cancer has spread and how quickly it might be growing.
How far has my cancer spread?
The stage of your cancer tells you whether it has spread outside the prostate and how far it has spread. You might need scans, such as an MRI, CT or bone scan, to find out the stage of your cancer.
Depending on the results, your cancer may be treated as:
- localised prostate cancer it’s contained inside the prostate
- locally advanced prostate cancer its started to break out of the prostate or has spread to the area just outside it
- advanced prostate cancer its spread from the prostate to other parts of the body.
Cambridge Prognostic Group
If you have localised or locally advanced prostate cancer, your doctor may talk to you about the risk of your cancer spreading outside the prostate. To work out your risk, your doctor will look at your PSA level, your Gleason score and the T stage of your cancer.
These three factors will place you in one of five categories that form the Cambridge Prognostic Group . This system is used to help your doctor decide which treatment options are suitable to you, based on your risk.
The five CPG categories are described below. If you have any questions about your CPG speak to your doctor or specialist nurse.
CPG 1
- Gleason score 6 , and
- PSA less than 10 ng/ml, and
- T stage of 1 or 2.
CPG 2
You will be in this group if you have a T stage of 1 or 2 and one of the following:
CPG 3
CPG 4
CPG 5
You May Like: Why Would An Enlarged Prostate Gland Interfere With Urination
Clinical Decision Support Systems For Diagnosis Of Prostate Cancer
Clinical Decision Support Systems offer patient-specific advice based on guideline recommendations to enhance the process of decision-making by physicians and other healthcare practitioners, improve safety, and facilitate evidence-based practice. A multifactorial decision support system describes a tool which improves the clinical decision-making process by utilizing clinical inputs for an individual patient to generate case-specific therapy advice .
Different decision support systems can be applied in PCa diagnostics to enhance early tumor detection, reduce overdiagnosis, and avoid unnecessary testing. These systems utilize several parameters including imaging, clinical, and biological features to improve detection and risk classification of PCa in a minimally invasive way, thereby maximizing individual treatment. mDSS for diagnostic interventions aim to detect, diagnose, or classify PCa using various methods. Several prediction tools are currently used in clinics to support PCa diagnostics including analysis of potential LN involvement, organ confinement, seminal vesicle involvement, and extracapsular extension as well as the risk of failure after treatment .
Outlook: Workflow Automation And Artificial Intelligence In Radiology
Within healthcare systems, AI will prospectively become a major driver of many applications, including medical diagnostics and imaging, risk management, and hospital management. AI enables the recognition of complex patterns in image data resulting in an automated quantitative assessment. Therefore, more accurate and standardized image assessment is possible when AI is integrated into the clinical workflow as a tool to assist physicians in their daily routine. The primary trigger for the implementation of AI in medical imaging has been the desire for greater efficacy and efficiency in clinical processes .
AI methods are often based on machine learning algorithms. Machine learning involves engineered features that are defined by human experts and interpreted in terms of mathematical equations and can thus be quantified by computer programs. These features are used as inputs to machine learning models, which are trained to classify diseases, thereby supporting clinical decision-making . Machine learning will generate novel algorithms which partly automate several aspects of the radiological workflow including image analysis, interpretation, and report creation to optimize decision support and therapy planning in the long term.
Don’t Miss: What To Expect With Prostate Radiation
Tnm Classification And Tumor Staging
TNM classification of PCa is based on the current UICC classification . The tumor stages T1â2 N0 M0 describe locally confined PCa, whereas locally advanced PCa encompasses the stages T3â4 N0/+âand M0. Therefore, locally advanced PCa includes tumors that extend the prostate capsule , infiltrate the seminal vesicles or neighboring structures , or expansions as locoregional LN metastases without distant metastases. Higher Gleason score distribution, a higher proportion of clinical T2 disease , as well as extraprostatic extension and the incidence of perineural invasion are associated with positive surgical resection margins and thus, higher biochemical recurrence rates with a worse prognosis, respectively . Within a prospective study investigating 1308 PCa patients, multivariate Coxâs proportional hazards regression analysis clearly outlined T3 stages as an independent pathological risk factor for BCR prediction in comparison to pathological T2 stages .
Extent Your Cancer Has Spread
If your cancer has spread outside of your prostate , there are two category measures to consider. These two measurements are commonly combined with your T-stage to form one TMN score.
N-Category: Determines if and how far the cancer has spread to your lymph nodes.M-Category: Determines if and how far the cancer has metastasized or spread to other organs.
Recommended Reading: How To Cure Prostatitis Without Antibiotics
What Combined Strategies In Pi
In the setting of suspicious imaging findings, it is accepted that MRI cannot negate the need for biopsy. Histopathological proof by targeted biopsies is necessary due to the high false-positive rate of MRI . If additional information can help to clarify further risk of suspicious lesions on MRI, the number of biopsies and false positive results can be reduced. Several strategies of combining additional information to MR imaging are under investigation. They may demonstrate a benefit in making a decision about which patient needs a biopsy and concurrently help avoid unnecessary biopsies. Studies on the added value in classifying further risk of PI-RADS category 3 lesions are limited.
Local Staging: Additional Anatomic Landmarks
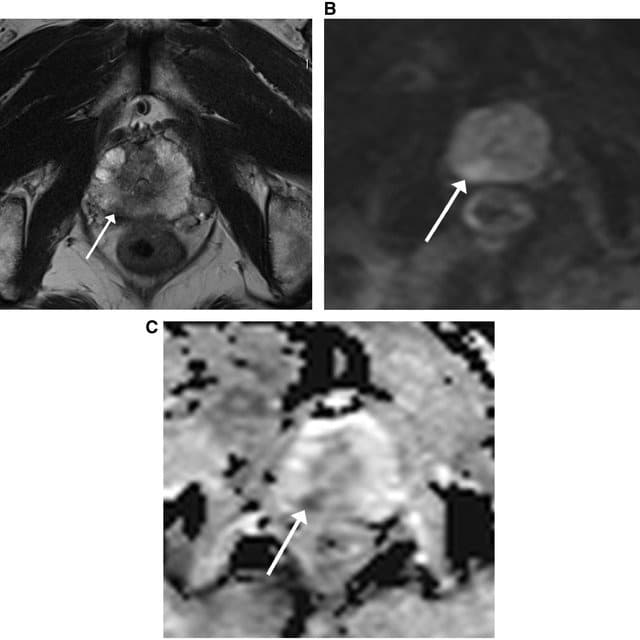
Clinically relevant anatomic landmarks should be scrutinized once a focal prostatic lesion is identified. Multiplanar assessment on T2W imaging is useful, as some relationships may not be evident in the axial plane.
| Key Local Staging Landmarks by Lesion Location |
| Base |
| Example of NVB Involvement | |
| Normal neurovascular bundle is visualized as a cluster of punctate/linear T2-hypointense foci |
Findings: Large right base PZ lesion with asymmetric T2 hypointense thickening along the right NVB , with corresponding restricted diffusion. Note the normal contralateral NVB .Surgery/Path: Right NVB resected at surgery. Path positive for EPE. |
Also Check: What Happens When You Have Your Prostate Removed
The Staging Grading And Prognosis Of Prostate Cancer
Staging
The tests completed by your specialist help work out whether you have prostate cancer and if it has spread to other parts of your body. This process is called staging. It helps you and your health care team decide which management or treatment option is best for you.
The most common staging system for prostate cancer is the TNM system. In this system, letters and numbers are used to describe the size of the tumour , whether the cancer has spread to nearby lymph nodes , and whether the cancer has spread to the bones or other organs, i.e. whether it has metastasised . The TNM scores are combined to work out the overall stage of the cancer, with higher numbers indicating larger size or spread.
| localised stages 12 | The cancer is contained inside the prostate. |
|---|---|
| locally advanced stage 3 | The cancer is larger and has spread outside the prostate to nearby tissues or nearby organs such as the bladder, rectum or pelvic wall. |
| advanced stage 4 | The cancer has spread to distant parts of the body such as the lymph glands or bone. This is called prostate cancer even if the tumour is in a different part of the body. |
Grade and risk category
The biopsy results will show the grade of the cancer. This is a score that describes how quickly the cancer may grow or spread.
Risk of progression
Prognosis
Prognosis means the expected outcome of a disease. You may wish to discuss your prognosis with your doctor, but it is not possible for anyone to predict the exact course of the disease.
Exam Preparation And Protocols
Don’t Miss: How Are Prostate Exams Performed
Stage 1 Prostate Cancer Treatment
Prostate cancer is found in the prostate gland only and is non-detectable by an imaging test or DRE physical examination. Older men, men who suffer other serious health issues or younger men may consider active surveillance due to the slow growth rate, possibility of never experiencing any symptoms or preference to delay treatment. However, radiation or proton therapy for stage 1 prostate cancer is often recommended to reduce the risk of cancer spreading, especially for those with higher Gleason scores and PSA levels. Almost 80% of the time, prostate cancer is discovered at this stage and the 5-year survival rate is nearly 100%.
You May Like: What Foods To Eat To Avoid Prostate Cancer
> > > 1 Bedtime Hack To Pee Like A Bull
An enlarged prostate can also be the cause of other problems. If the enlarged prostate is causing symptoms, the best treatment would be a natural remedy. In the meantime, there are treatments for a wide range of conditions that cause a man to experience pain. A common surgical procedure involves an electric loop, laser, or electro-stimulation. The procedure is a safe and effective option for treating enlarged or symptomatic BPH.
Don’t Miss: Complications Of Radiation For Prostate Cancer
Use In Men Who Might Have Prostate Cancer
The PSA blood test is used mainly to screen for prostate cancer in men without symptoms. Its also one of the first tests done in men who have symptoms that might be caused by prostate cancer.
PSA in the blood is measured in units called nanograms per milliliter . The chance of having prostate cancer goes up as the PSA level goes up, but there is no set cutoff point that can tell for sure if a man does or doesnt have prostate cancer. Many doctors use a PSA cutoff point of 4 ng/mL or higher when deciding if a man might need further testing, while others might recommend it starting at a lower level, such as 2.5 or 3.
- Most men without prostate cancer have PSA levels under 4 ng/mL of blood. Still, a level below 4 is not a guarantee that a man doesnt have cancer.
- Men with a PSA level between 4 and 10 have about a 1 in 4 chance of having prostate cancer.
- If the PSA is more than 10, the chance of having prostate cancer is over 50%.
If your PSA level is high, you might need further tests to look for prostate cancer.
To learn more about how the PSA test is used to look for cancer, including factors that can affect PSA levels, special types of PSA tests, and what the next steps might be if you have an abnormal PSA level, see Screening Tests for Prostate Cancer.
Grade And Risk Category
The biopsy results will show the grade of the cancer. This is a score that describes how quickly the cancer may grow or spread.
For many years, the Gleason scoring system has been used to grade the tissue taken during a biopsy. If you have prostate cancer, youll have a Gleason score between 6 and 10. A new system has been introduced to replace the Gleason system. Known as the International Society of Urological Pathologists Grade Group system, this grades prostate cancer from 1 to 5 .
Risk of progression
Based on the stage, grade and your PSA level before the biopsy, localised prostate cancer will be classified as having a low, intermediate or high risk of growing and spreading. This is known as the risk of progression. The risk category helps guide management and treatment.
Grading prostate cancer
| High risk. The cancer is likely to grow aggressive. |
Recommended Reading: What Is The Cost Of Radiation Treatment For Prostate Cancer
