What Is A Hypoechoic Lesion
A hypoechoic lesion is an abnormal area that can be seen during an ultrasound examination because it is darker than the surrounding tissue. Such abnormalities can develop anywhere in the body and do not necessarily indicate cancer. Blood tests, biopsies, and further radiological studies may be required to determine the composition of a hypoechoic lesion, sometimes referred to simply as a lesion.
Detecting a Hypoechoic Lesion
During an ultrasound examination, a technician applies a handheld device known as a transducer to the area of the body requiring assessment. The transducer emits high frequency sound waves that are reflected back toward the device when they contact internal structures. A black and white image forms on a monitor, based on the intensity of the echoes. Radiologists call brighter images from highly reflective surfaces hyperechoic while areas that are less reflective appear as darkened regions and are said to be hypoechoic.
Common Hypoechoic Lesions
What To Expect After The Biopsy
After the biopsy, you can resume your usual activities. However, your doctor might advise you not to sit for extended periods and avoid lifting heavyweight.
Talk to your doctor if you experience abundant bleeding, high fever, and flu-like symptoms.
Your urologist may schedule a follow-up to see how youre doing.
They may order a blood culture and urine culture to rule out infections after a biopsy.
Careful monitoring is always recommended, even if the biopsy result is negative.
Thus, you may still need to go back with your doctor every year for a prostate specific antigen test, a digital rectal exam, and other evaluations.
Overlap With Benign Conditions
MRI derived parameters are reflective of pathologically determined characteristics of prostate cancer, however, there is great overlap with benign conditions, such as benign prostate hyperplasia, inflammation or fibrosis. These benign abnormalities have been implicated as sources of false-positive MR imaging findings or poor radiologic-pathologic volumetric correspondence . These issues are at most applicable to PI-RADS 3 lesions, as shown by the high rate of benign outcomes of targeted biopsies: prostate cancer was not detected in respectively 61% and 71% in men with first biopsies and previous negative biopsies .
Read Also: Prostate Cancer And Testosterone Levels
C Role Of Mpmri In Evaluating Regional Lymphatics
Currently available imaging modalities for the evaluation of lymph nodes in patients with intermediate to high risk prostate cancer have high specificity and accuracy but only low to moderate sensitivity. mpMRI appears to be equivalent to computerized tomography and positron emission tomography in this regard.
Although we are not aware of any contemporary direct comparisons of CT and mpMRI for pelvic lymph node metastases, a meta-analysis published in 2008 suggested no meaningful difference in operating characteristics, although both were notably suboptimal with pooled sensitivity of 0.39 0.42 and pooled specificity of 0.82.111
Von Below et al. showed that mpMRI DWI had a 90% specificity, 55% sensitivity, and 72.5% accuracy for lymph node metastasis in 40 patients with intermediate- and high-risk prostate cancer, 20 of whom had histologically-proven lymph node positive disease. The true-positive patients had significantly more involved lymph nodes , with larger diameter compared with the false-negative group.115 Vallini et al. showed that using 3.0T DWI mpMRI with a multiple b-value spin echo-echo planar imaging sequence may help distinguish benign from malignant pelvic lymph nodes in patients with prostate cancer.116
Key Points
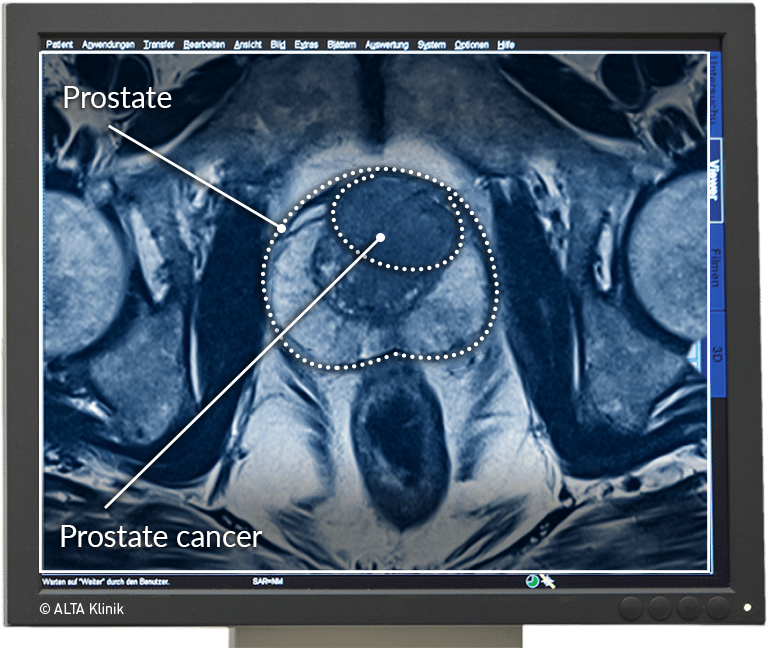
Malignant Focal Prostate Lesions
Prostate cancer is a common disease and an important health issue for men worldwide. The diagnosis and management of prostate cancer is highly complex, stemming from the uncertain natural history of the disease and its unpredictable biologic behavior. There is a high prevalence of the disease autopsy series have revealed small prostate cancers in as many as 29% of men between ages 30 and 40 and 64% of men between ages 60 and 70. However, a high proportion of prostate cancer fails to develop into clinically significant symptomatic cancer. There is no perfect method to determine which patients will have disease that will progress. Factors such as a high PSA level, Gleason score, and stage are all useful for predicting outcome, but algorithms that combine stage, grade, and PSA level to predict pathologic stage or prognosis perform better than these individual factors alone. Imaging plays an important contributory role in the management of prostate cancer.
Don’t Miss: How Does Prostate Cancer Start
What Gets Stored In A Cookie
This site stores nothing other than an automatically generated session ID in the cookie no other information is captured.
In general, only the information that you provide, or the choices you make while visiting a web site, can be stored in a cookie. For example, the site cannot determine your email name unless you choose to type it. Allowing a website to create a cookie does not give that or any other site access to the rest of your computer, and only the site that created the cookie can read it.
Prostate Cancer No Biopsy In Case Of A Normal Mri Summary:
Sigrid V. Carlsson, MD, PhD, MPH, and Gerald L. Andriole, Jr., MD, discuss the pros and cons of omitting biopsy in patients with abnormal PSA levels and a negative MRI. While avoiding standard biopsy can mitigate serious complications, the data may not support full confidence in MRIs detection quality.
Also Check: What Does Gleason Score Mean In Prostate Cancer
Cm Lesion On Prostate 1 Introduction
The derived LOAEC for systemic effects was 32 ppm taking into account the decrease in sperm motility for male mouse exposed to vapour concentrations of 32 ppm and higher concentration levels.
All animals survived to the end of the study. The absolute weights of the liver, right kidney, and thymus of ppm males heart, liver, and right kidney of ppm females and thymus of 62 and ppm females were significantly less than those of the chamber controls.
The relative weights of the heart, right kidney, lung, and right testis of ppm males and the lung of ppm females were significantly greater than those of the chamber controls. Except for a slight 0. Histopathologic changes were noted primarily in the nasal cavity and involved both the respiratory and olfactory epithelium of males and females principally in the 62 or ppm groups.
These lesions included suppurative inflammation, squamous metaplasia of the respiratory epithelium, olfactory epithelial atrophy, and necrosis of the turbinates. Significant olfactory epithelial atrophy was already observed after treatment with 32 ppm.
A NOAEC of 16 ppm for local effects was derived based on the observed nonneoplastic lesions of the mouse nose. The derived LOAEC for systemic effects was 32 ppm taking into account the decrease in the sperm motility for male mouse exposed to vapour concentrations of 32 ppm and higher concentration levels.
Also Check: Prostate Cancer Center Of New Jersey
When To Order An Mri In The Initial Evaluation And Management Of Prostate Cancer
This article summarizes the current role of multiparametric MRI in the diagnosis, risk assessment, and treatment of prostate cancer.
Prostate cancer remains the only solid tumor diagnosed using transrectal ultrasoundguided sampling of the gland, and not an image-based, lesion-directed approach. This technique has limitations in that it underdiagnoses clinically significant disease and overdiagnoses indolent tumors resulting in overtreatment of patients. Technical advances in MRI in the last decade have made this method the preferred imaging modality for prostate anatomy and for risk assessment of prostate cancer. As of 2018, the indications for MRI in the diagnosis and risk assessment of prostate cancer have expanded from preoperative evaluation to the pre-biopsy setting, as well as for surveillance protocols. This article summarizes the current role of multiparametric MRI in the diagnosis, risk assessment, and treatment of prostate cancer.
Don’t Miss: How High Is Psa In Prostate Cancer
Prostate Mri Can Help Differentiate Between Harmless And Aggressive Cancers Preventing The Overdiagnosis Of Low
There are two forms of prostate cancer: aggressive and harmless. Fortunately, out of all prostate cancer cases, only a fraction will be aggressive and clinically significant. The majority will never impact the well-being or life expectancy of a patient.
Prostate MRI can help reduce the number of men who are over-diagnosed by 5%.
A prostate MRI scan enables radiologists to better differentiate between aggressive and harmless cancers by providing information about a tumors size, density, and proximity to the bloodstream. One study comparing prostate MRI to biopsy found MRI scans to correctly diagnose 93% of tumors, whereas biopsy correctly diagnosed only 48%. Identifying non-threatening forms of prostate cancer helps decrease the risk of overdiagnosis and overtreatment.
But do keep in mind that MRIs can be complex images for radiologists to interpret. Coupling a prostate MRI with a subspecialty second opinion from a fellowship-trained radiologist can help maximize the advantages and efficacy of the screening. This can be done completely online and is especially recommended for scans that indicate the possibility of aggressive prostate cancer.
CONNECT WITH A SPECIALIST
Take Charge of Your Health
Get a second opinion from a radiology specialist in 3 easy steps.
Medical History And Physical Exam
If your doctor suspects you might have prostate cancer, you will be asked about symptoms you are having, such as any urinary or sexual problems, and how long you have had them. You might also be asked about possible risk factors, including your family history.
Your doctor will also examine you. This might include a digital rectal exam , during which the doctor inserts a gloved, lubricated finger into your rectum to feel for any bumps or hard areas on the prostate that might be cancer. If you do have cancer, the DRE can sometimes help tell if its only on one side of the prostate, if its on both sides, or if its likely to have spread beyond the prostate to nearby tissues. Your doctor may also examine other areas of your body.
After the exam, your doctor might then order some tests.
Also Check: Stage Two Prostate Cancer Prognosis
About Dr Dan Sperling
Dan Sperling, MD, DABR, is a board certified radiologist who is globally recognized as a leader in multiparametric MRI for the detection and diagnosis of a range of disease conditions. As Medical Director of the Sperling Prostate Center, Sperling Medical Group and Sperling Neurosurgery Associates, he and his team are on the leading edge of significant change in medical practice. He is the co-author of the new patient book Redefining Prostate Cancer, and is a contributing author on over 25 published studies. For more information, contact the Sperling Prostate Center.
Search the spc blog
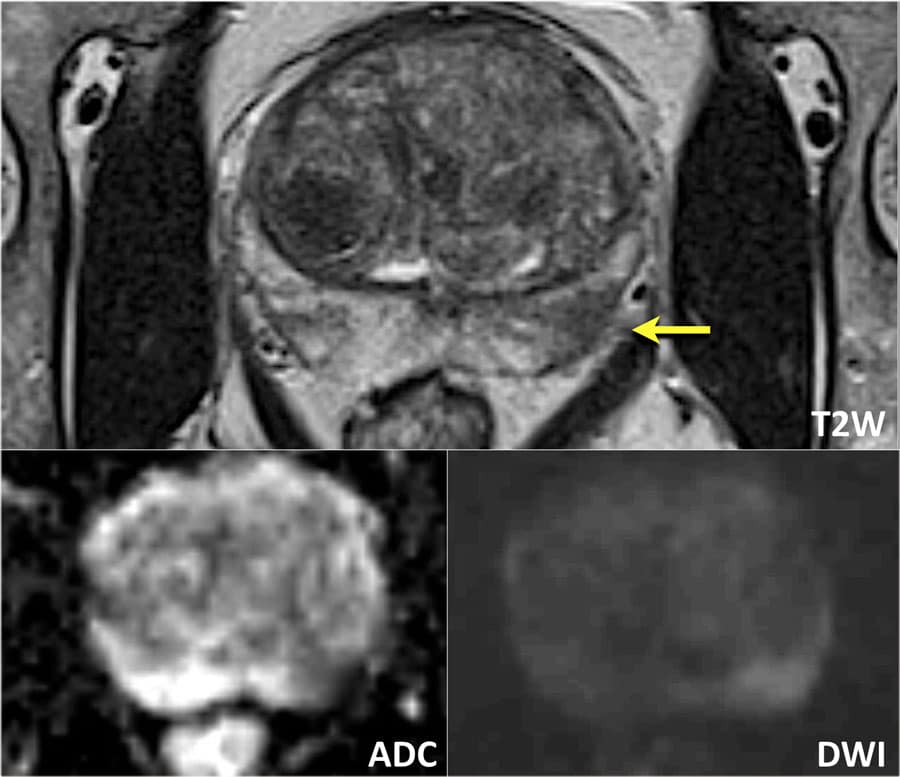
Role Of Dce Mriand Status Of Biparametric Mri
One area of attention in prostate MRI is the relatively narrow role of DCE MRI within PI-RADSv2, largely being applied for characterization of indeterminate lesions in the peripheral zone . Upon release of PI-RADSv2, several subsequent studies evaluated the role of DCE MRI in prostate cancer diagnosis. Greer et al. evaluated the validity of the dominant sequence paradigm in a 58-patient retrospective nine reader study. Their results indicated that the probability of cancer detection for PI-RADSv2 category 2, 3, 4, and 5 lesions was 15.7%, 33.1%, 70.5%, and 90.7%, respectively. DWI outperformed T2W in the PZ . T2W performed better but did not clearly outperform DW imaging in the transition zone . Lesions classified as PI-RADSv2 category 3 at DWI and as positive at DCE imaging in the PZ showed a higher probability of cancer detection than did DCE-negative PI-RADSv2 category 3 lesions . The addition of DCE imaging to DWI in the PZ was beneficial , with an increase in the probability of cancer detection of 15.7%, 16.0%, and 9.2% for PI-RADSv2 category 2, 3, and 4 lesions, respectively.20
Also Check: Can Colon Cancer Spread To Prostate
Prostate Mri Can Help You Avoid Unnecessary Biopsy
Prostate biopsies are used to confirm cancer in high-risk patients suspected to have aggressive prostate cancer. Uncomfortable and invasive, men undergoing the procedure are extremely prone to complications like antibiotic-resistant infections and sepsis. Its estimated that 18% of patients experience some sort of complication, while as many as 4% develop an infection requiring hospital care.
27% of the one million prostate biopsies performed each year are unnecessary.
Typically, a biopsy will be recommended to a patient for one of two reasons: they tested high for levels of the PSA protein, or, the results from a digital rectal exam show they may have prostate cancer. The issue here is that PSA tests are not always accurate.
A males PSA level can be affected by a number of other factors, such as recent sexual activity, an enlarged prostate, and prostatitis. Even a long bicycle ride can cause levels to spike. This leaves a lot of room for false-positives – which lead to unnecessary biopsies.
Prostate Tb Abscess In A Patient With Bladder Tcc After Intravesical Instillation Of Bcg
Adjuvant intra-vesical immunotherapy with BCG for bladder transitional cell carcinoma can lead to a rare complication of tuberculous infection in the prostate via haematogenous spread and direct extension which can cause a prostate abscess .
The granulomatous reaction that occurs in prostate tissues following the topical instillations of BCG after resection of bladder cancer can present MRI features similar to prostate cancer . It appears as an ill-defined region with moderate contrast enhancement, diffusion restriction and very low ADC values due to the high cellular density. These are a well-recognised cause of false positive MRI. However, frank abscess formation related to BCG is rare with only a handful of cases described in the literature. History and biochemical correlation are important to consider this as a differential diagnosis and a biopsy may be needed to confirm .
Fig. 7
Prostate abscessa, b Axial T2W images show left lateral bladder wall thickening and heterogeneous but predominantly low T2 signal in the left prostate , respectively. c Post-contrast, the lesion demonstrates strong peripheral contrast enhancement and on DWI/ ADC in d, e, respectively, the central element of the left prostate lesion shows restricted diffusion with a very low ADC value
You May Like: Does Super Beta Prostate Work
American Guidelines Say No
Here in the United States, professional organizations have also expressed their reservations: the American Urological Association, for instance, warns in its current guidelines that the risk of missing clinically significant prostate cancer on a negative mpMRI raises persistent concerns.
During a recorded conversation hosted by Grand Rounds in Urology, Dr. Sigrid Carlsson, a physician-epidemiologist from the Memorial Sloan Kettering Cancer Center in New York, acknowledged that while men would understandably want to avoid a biopsy, radiologists vary significantly in how well or accurately they read mpMRIs, and miss rates can range up to 20%. The false negative diagnoses occur most frequently among radiologists who are just learning how to interpret the scans, and for that reason, she said, We cant avoid biopsy if the mpMRI is negative because the miss rate is so high.
Dr. Anthony DAmico, a professor at Harvard Medical School and an author on the AUA guidelines, gave the same reason to back his view that a standard 12-core biopsy should still be undertaken despite negative mpMRI readings.
The decision to biopsy or not could be aided with better diagnostic tools, and one cited repeatedly is PSA density, or the total amount of PSA in blood divided by the prostate volume. High PSA densities denote higher risk, and when combined with mpMRI findings, could enable patients to make a more informed choice.
About the Author
How Fast Does Prostate Cancer Spread To The Bones
Early detection can catch prostate cancer even before there are any symptoms. Some types of prostate cancer grow very slowly.
There are four main stages of prostate cancer. Within each stage, the cancer is graded based on factors like the size of tumor, prostate-specific antigen level, and other clinical signs.
If the cancer has spread to the bones, its considered to be the most advanced, or stage 4.
Newer lab tests look at the genes inside cancer cells. This can provide more information on how quickly the prostate cancer may progress.
Theres also a grading system known as the Gleason system, which assigns the cancer into a grade group based on how closely it resembles normal tissue.
During the biopsy to diagnose prostate cancer, the cells are closely examined. The more abnormal cells that are in the biopsy sample, the higher the Gleason score and grade group.
When more abnormal cells are present, the cancer is more likely to spread quickly.
Read Also: Prostate Cancer And Lung Cancer
Recommended Reading: How Many Chemo Treatments For Prostate Cancer
Features Of Pin Cells
Basal cellspecific monoclonal antibodies directed against highmolecular weight keratin are used to identify HGPIN cells. Normal prostatic epithelial cells are consistently stained with these antibodies, showing a continuous, intact, circumferential basal cell layer. Cancer cells have lost their receptors for these antibodies.
Basal cell disruption affects 56% of patients with HGPIN and is usually found in glands adjacent to invasive cancer. The degree of disruption correlates with HGPIN. More than one third of the basal cell layer is lost in 52% of foci that contain HGPIN.
In persons with HGPIN and in many with low-grade cancer, the basement membrane that surrounds the prostatic glands remains intact. The expression of collagenase type 4 in PIN and associated cancer cells is abnormally high. The presence of collagenase type 4 and other enzymes is associated with a degradation of the basement membrane, allowing cell invasion into the stroma. Concurrently, the basal cell layer is diminished. This seems to occur primarily at sites of glandular outpouching.
Increased angiogenesis with an increased number of microvessels is associated with the progression of HGPIN to cancer. The microvessels in HGPIN are shorter than those in benign epithelium and have irregular contours and open lumens, an increased number of endothelial cells, and a greater distance from the basement membrane.
Also Check: Best Cancer Center For Prostate Cancer
