What Is An Mri Fusion Biopsy
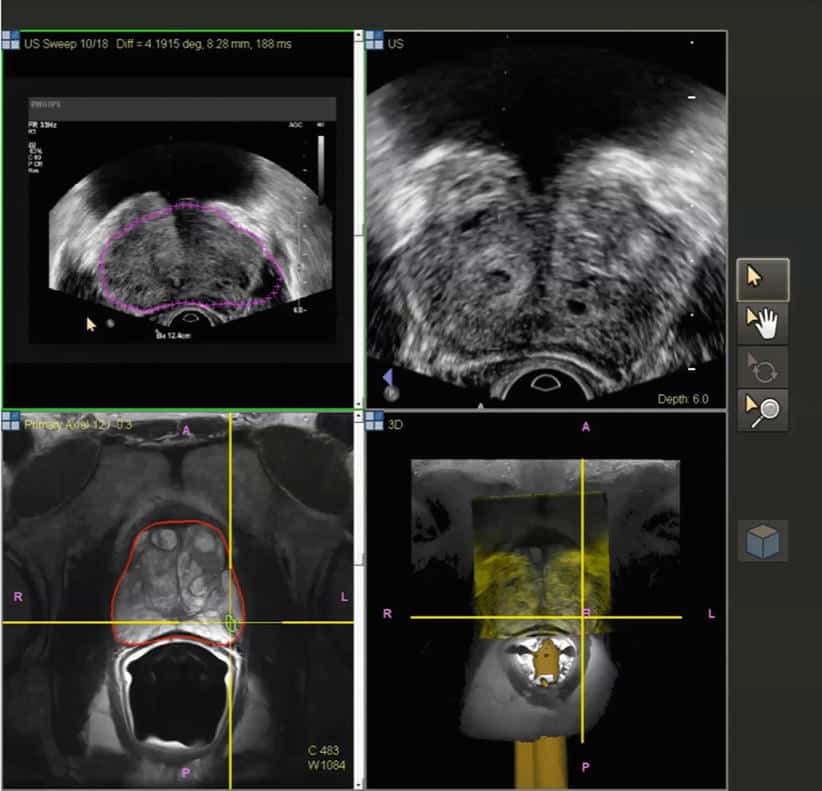
An MRI fusion biopsy is one of the most valuable tools for diagnosing and staging prostate cancer. This advanced procedure combines imaging technology with targeted tissue sampling for ultimate precision and accuracy. During an MRI fusion biopsy in the Jacksonville, FL area, patients will first have an MRI performed to identify the exact locations from which tissue samples should be taken. On the day of the biopsy, Dr. Ali Kasraeian will use ultrasound imaging along with the MRI image results to guide the needle to the precise locations that need to be biopsied.
Prostate 3t Multiparametric Mri
Experts agree that MRI is the most sensitive imaging technique in relation to other imaging technologies at this time. Todays features include a number of parameters captured by a powerful 3 Tesla magnet that reveal much more than just prostate anatomy, enabling visual definition of even small prostate cancer tumors:
- Diseased tissue shows up as anatomical differences See Fig. 2a
- The movement of water molecules in tumor cells, different from normal cells See Fig. 2b
- The presence of certain chemicals in tumor cells, unlike normal cells See Fig. 2c
- Changes in the uptake and washout of contrast agents, another specific way to characterize cancer cells See Fig. 2d
In addition to these multiparametric indicators of a cancer, our powerful 3T magnet provides very high resolution of tumors.
Studies designed to correlate tumors identified by mpMRI in pre-prostatectomy patients confirm the accuracy of the MRI images when read by an experience radiologist, then compared with the surgically removed prostate specimens. According to an authoritative Dutch center, Multiparametric -MRI has been shown to be highly accurate in detecting and localizing intermediately aggressive and highly aggressive cancers. However, they caution that the experience of the radiologist conducting prostate MRI is crucial to how well images are captured and interpreted according to the highest standards.
Fig. 2a: T2 weighted images show suspected tumor activity
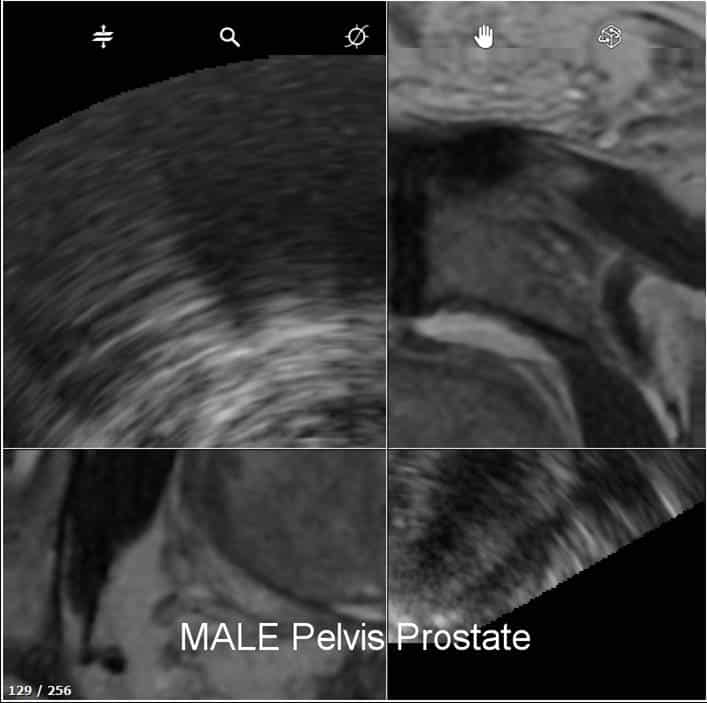
Performing An Mri Fusion Biopsy
The procedure is called an MRI fusion biopsy because it fuses together results from an MRI scan and an ultrasound-guided biopsy. The first step in the process is to perform an MRI scan. A device called an endorectal coil is inserted into the rectum to produce internal images. A special contrast dye is administered by IV towards the end of the exam. The images will then be reviewed and any suspicious lesions will be marked. If no targets are identified with the MRI, the biopsy part of the procedure may not be necessary.
However, if suspicious areas are identified, the second step in the process is the biopsy itself. A urologist will used the marked images from the MRI. These images are fused with real-time images of the area being targeted for testing to improve the accuracy of needle placement for the collection of tissue samples. A standard non-targeted 12-core transrectal ultrasound biopsy may also be performed along with the targeted biopsy. Prior to the biopsy, patients are usually advised to drink a few glasses water since a full bladder makes it easier to view the prostate.
You May Like: What Blood Test Checks For Prostate Cancer
What Does The Equipment Look Like
Ultrasound equipment:
Ultrasound scanners consist of a console containing a computer and electronics, a video display screen and a transducer or probe that is used to do the scanning. The transducer sends out inaudible high frequency sound waves into the body and then listens for the returning echoes. The principles are similar to sonar used by boats and submarines.
The ultrasound image is displayed on a video screen that looks like a computer or television monitor. The resulting image is based on the amplitude and frequency of the signal. The ultrasound image makes an image taking into account signal travel time, tissue composition, and type of body structure through which the sound travels.
The ultrasound probe used in prostate biopsies is about the size of a finger. Once the probe is placed in the rectum, the biopsy is performed with a spring-driven needle core biopsy device, or biopsy gun. The handheld device includes a long but very thin needle specially designed to open inside the prostate, take the sample and then close.
MRI equipment:
The traditional MRI unit is a large cylinder-shaped tube surrounded by a circular magnet. You will lie on a table that slides into the center of the magnet.
Getting The Results Of The Biopsy
Your biopsy samples will be sent to a lab, where they will be looked at with a microscope to see if they contain cancer cells. Getting the results usually takes at least 1 to 3 days, but it can sometimes take longer. The results might be reported as:
- Positive for cancer: Cancer cells were seen in the biopsy samples.
- Negative for cancer: No cancer cells were seen in the biopsy samples.
- Suspicious: Something abnormal was seen, but it might not be cancer.
If the biopsy is negative
If the prostate biopsy results are negative , and the chance that you have prostate cancer isnt very high based on your PSA level and other tests, you might not need any more tests, other than repeat PSA tests sometime later.
But even if many samples are taken, biopsies can still sometimes miss a cancer if none of the biopsy needles pass through it. This is known as a false-negative result. If your doctor still strongly suspects you have prostate cancer , your doctor might suggest:
- Getting other lab tests to help get a better idea of whether or not you might have prostate cancer. Examples of such tests include the Prostate Health Index , 4Kscore test, PCA3 tests , and ConfirmMDx. These tests are discussed in Whats New in Prostate Cancer Research?
- Getting a repeat prostate biopsy. This might include getting additional samples of parts of the prostate not biopsied the first time, or using imaging tests such as MRI to look more closely for abnormal areas to target.
Prostate cancer grade
Gleason score
You May Like: Abiraterone Prostate Cancer Life Expectancy
How Often Do Prostate Biopsies Find Cancer
The likelihood that a prostate biopsy will detect cancer depends greatly on the pre-biopsy profile of the person undergoing the procedure. If you have a high PSA score and/or suspicious changes to your prostate, a biopsy is more likely to detect cancer than if you have no significant risk factors or indications that you may have cancer.
This is why its important to have a thorough conversation with your doctor about why they are recommending a biopsy. A small 2015 study found a positivity rate of 52%, which the researchers noted was higher than most published averages.
In recent years, the combination of an MRI-guided and TRUS-guided biopsy is becoming more popular.
The combination of these the two imaging technologies, known as a , allows the doctor to see combined images of the prostate that are more detailed than MRI or ultrasound alone.
According to a , prostate biopsy is the gold standard screening for prostate cancer, and the combination of MRI and TRUS has advantages over traditional biopsy procedures.
A separate 2020 review suggests that TRUS-guided biopsies without MRI tend to result in an excessive amount of findings associated with non-significant disease and that they under-detect clinically significant cancer findings.
Apart from biopsies, your doctor may turn to other tests to detect prostate cancer or the possibility of cancer. These other screenings include:
Fusion Of Ultrasound And Mri
Fusion is a fluid process that involves de-forming an image and warping it to blend with the form of another. For medical purposes in the prostate, fusion merges previously captured MRI images with live TRUS images while the ultrasound wand is inserted. Only a very small number of U.S. urologists have the necessary knowledge, equipment and software to do fusion, and there are several fusion device manufacturers in the marketplace that may not be equal in performance.
How does it work? Prostate fusion imaging is usually done in the urologists office to help identify the target area for the biopsy. The urologist must be specially trained to read prostate MRI and identify the area of interest . The urologist must also segment or input the prostate outline into the computer to facilitate matching MRI and TRUS shapes. Special software is necessary that can recognize both types of images, assign coordinates to each type, and match the images coordinate-by-coordinate. This is called image registration or co-registration, and it overlays the live TRUS image onto the static MRI image. The result a synthetic 3D image of the patients gland that is quite accurate, but not perfect due to possible error artifacts such as patient movement, inaccurate segmentation, etc. The final 3D image can be manipulated on the computer screen so the urologist can view it from every angle, and the suspicious area is highlighted within the image.
Recommended Reading: How Likely Is It For Prostate Cancer To Spread
What Is Fusion Biopsy
We asked Edward D. King, MD, vice-president of Ocalas Advanced Urology Institute about this state-of-the-art new treatment for prostate patients.
Dr. King says, Transrectal ultrasoundMRI prostate fusion biopsy is the new standard of care for the detection of prostate cancer. The only definitive diagnosis comes from biopsy, and these only work if cancer cells are detected. Until now, traditional approaches were notoriously hit or miss.
A PSA blood test as well as a digital rectal exam performed by a patients personal physician, feeling for any obvious prostate abnormalities such as areas if induration or nodularity are the first tests.
The Prostate-Specific Antigen is a protein produced by both healthy and malignant prostate glands and measures the amount of that protein in the blood. A PSA of 4.0 or less is considered normal. Test results above 4.0 may indicate prostate cancer. But even that can be inconclusive. Fully 10 percent of patients who present with prostate cancer have normal-ranged PSAs readings.
Next, using a transrectal ultrasound probe for guidance, a biopsy needle is inserted into the prostate and biopsies performed in a systematic pattern with the hope that tissue samples provide answers. Unfortunately, 15 to 20 percent of the areas of cancer can be missed.
What Are The Advantages Of An Mri
Research has shown that using an MRI image to guide a biopsy improves detection of prostate tumors that require treatment, while finding fewer tumors that are called biologically insignificant. This means that they do not need any immediate treatment and are not likely to pose a threat to the patient. Because using an MRI image gives doctors better information and reduces the chance that a serious tumor will be missed, it should also mean that patients with blood-test results that suggest possible prostate cancer are less likely to need repeat biopsies because the first one may have produced a false negative.
Don’t Miss: If Prostate Cancer Spreads To Lymph Nodes
Magnetic Resonance Imaging And Ultrasound Fusion Guided Prostate Biopsy
The MRI/US Fusion Guided Prostate Biopsy combines magnetic resonance imaging and ultrasound technologies, enabling a targeted biopsy that is able to focus directly on suspicious areas of the prostate, unlike the traditional method. This advanced screening technique is also able to detect prostate cancer much sooner than with previous tests and marks one of the most significant advances in prostate screening in 30 years. It is expected to be especially helpful among men with a history of negative biopsies who are still suspected of having cancer due to persistently abnormal lab results, patients with enlarged prostates, and men who are being monitored based on certain test results. When cancer is detected, the technique provides a more accurate understanding of the disease, which allows physicians to offer better counsel to patients, who in turn can make more informed decisions regarding their care.
We Do Not Need A Rectal Coil With Our Elition 30t System And Its High Quality Gradients Providing High Quality Imaging
Many patients have had prior MRIs, which they disliked, because its noisy, uncomfortable, boring, and the gantry is tight. And invariably, after we scan them in our Elition, most of them say, Hey, this wasnt as bad as I thought it was going to be. I would say that patients are pleasantly surprised that the scan was quicker than theyve experienced in the past the immersive experience is pleasant for them, and the bore seems more open than they remember. The Elition system is definitely a step up in terms of patient comfort and frankly in imaging too.
When asked if he would recommend 3.0T for prostate imaging, Dr. Steiner says: Undoubtedly! When I look back at our prior scans that were done on a 1.5T, then the quality, the conspicuity of lesions and my diagnostic confidence are unquestionably improved with the Elition 3.0T. We had looked at all major vendors and selected Philips, because I thought Philips excels in technology as well as the ability to use ExamCards and the ability to cross-train our technologists.
Read Also: Brca Testing For Prostate Cancer
Overcoming Shortcomings Of A Traditional Biopsy
With a traditional biopsy, ultrasound is usually used to help with the accuracy of needle placement. However, the resulting images are sometimes not clear enough to distinguish cancerous tissue from normal tissue, which can make it difficult to zero in on the right tissue to collect for the biopsy. These so-called random biopsies sometimes miss harmful tumors or identify ones that are treated unnecessarily. An MRI scan alone cant be used to diagnose cancer, but the images produced make it easier to identify suspicious areas with better accuracy.
What Is A Biopsy
A biopsy is a procedure that removes a sample of tissue or cells for study and are most commonly used to look for cancer.
Prostate biopsies are done with a biopsy needle that can be positioned with the assistance of ultrasound images to get samples for testing.
Your doctor might decide you need a prostate biopsy based on the results of a blood test that measures your level of PSA . A high PSA result might point to cancer, but there are other things such as non-cancerous enlargement or infection that cause PSA to rise. Tests that measure derivatives of PSA such as OPKO 4k and Prostate Health Index may be more accurate than PSA in assessing your risk for having a cancer that needs treatment.
Don’t Miss: Can Prostate Cause Frequent Urination
What Will I Experience During And After The Biopsy
If you receive IV contrast for the MRI-guided procedure, you may feel coolness and a flushing sensation for a minute or two following the injection. The IV needle may cause some discomfort when the doctor inserts it and you may have some bruising when they remove it.
Rarely, patients may experience side effects from MR contrast material, such as nausea and local pain, hives, itchy eyes, or other reactions. If you have allergic symptoms, a radiologist or other doctor will be available for immediate assistance.
When the doctor inserts the ultrasound probe or endorectal coil into the rectum, you will feel pressure and may have some temporary discomfort.
You will hear a clicking noise when the biopsy needle samples the prostate and you may feel a stinging or burning sensation in the area.
Some patients find it uncomfortable to remain still during an MRI. Others experience a sense of being closed-in . Sedation is available for patients who anticipate anxiety.
If you feel heating on your skin at any time during MR imaging, tell the MR technician so they can closely examine the area.
Some patients experience a small amount of bleeding from the rectum or perineum immediately after the biopsy. If this does occur, it will cease with gentle pressure.
If you did not receive sedation, no recovery period is necessary. Light general anesthetic or sedation may leave you feeling groggy for a day or so.
Rapid Scanning Time And More Patientcomfort With Elition
Dr. Steiner currently performs all prostate MRI examinations on the Ingenia Elition 3.0T scanner. Previously, our scans were over 45 minutes per patient. However, with Elition and Compressed SENSE we have now decreased our scanning time to approximately 25 to 28 minutes, with more patient comfort, says Dr. Steiner. We have also achieved significantly improved resolution and more consistent parameters for interpretation. VitalEye, VitalScreen and other workflow features all add significantly to the patient experience as well as patient throughput.
Don’t Miss: 3 Signs Of Prostate Cancer
Use In Men Who Might Have Prostate Cancer
The PSA blood test is used mainly to screen for prostate cancer in men without symptoms. Its also one of the first tests done in men who have symptoms that might be caused by prostate cancer.
PSA in the blood is measured in units called nanograms per milliliter . The chance of having prostate cancer goes up as the PSA level goes up, but there is no set cutoff point that can tell for sure if a man does or doesnt have prostate cancer. Many doctors use a PSA cutoff point of 4 ng/mL or higher when deciding if a man might need further testing, while others might recommend it starting at a lower level, such as 2.5 or 3.
- Most men without prostate cancer have PSA levels under 4 ng/mL of blood. Still, a level below 4 is not a guarantee that a man doesnt have cancer.
- Men with a PSA level between 4 and 10 have about a 1 in 4 chance of having prostate cancer.
- If the PSA is more than 10, the chance of having prostate cancer is over 50%.
If your PSA level is high, you might need further tests to look for prostate cancer.
To learn more about how the PSA test is used to look for cancer, including factors that can affect PSA levels, special types of PSA tests, and what the next steps might be if you have an abnormal PSA level, see Screening Tests for Prostate Cancer.
