What Is Urinary Incontinence And How Is It Related To Prostate Cancer Surgery
Urinary incontinence is the loss of the ability to control urination . Urinary incontinence sometimes occurs in men who’ve had surgery for prostate cancer.
If youve had prostate cancer surgery, you might experience stress incontinence, which means you might leak urine when you cough, sneeze or lift something that is heavy. This happens because of stress or pressure on the bladder. There is also a type of incontinence that is called urge incontinence. When this happens, you are hit with a sudden need to urinate right away and have leakage before you can make it to the bathroom.
Ive Just Had Surgery And Im Leaking Urine What Can I Do
Even if youve been told you may leak urine after surgery it can still be quite a shock when it happens. Wearing absorbent pads or underwear can stop you wetting your clothes. They are often very discrete and no one would know that youre wearing them.
They can be reusable and washed with your usual laundry or disposable to stick into your underwear. They come in many different sizes and shapes and hold different amounts of urine. You can also get absorbent pants to wear instead of your underwear.
Some hospitals and GP surgeries will prescribe free pads. But this will depend on the area and you might have to pay for them yourself. Your GP, nurse or incontinence team should be able to tell you whether this is the case in your area.
If not, you can buy pads from supermarkets or chemists, or order directly from the manufacturer some may send you an initial sample for free. Some websites, such as the Incontinence Supermarket, sell pads VAT free, so shop around to get the best deal.
How Can Prostate Surgery Affect Urination
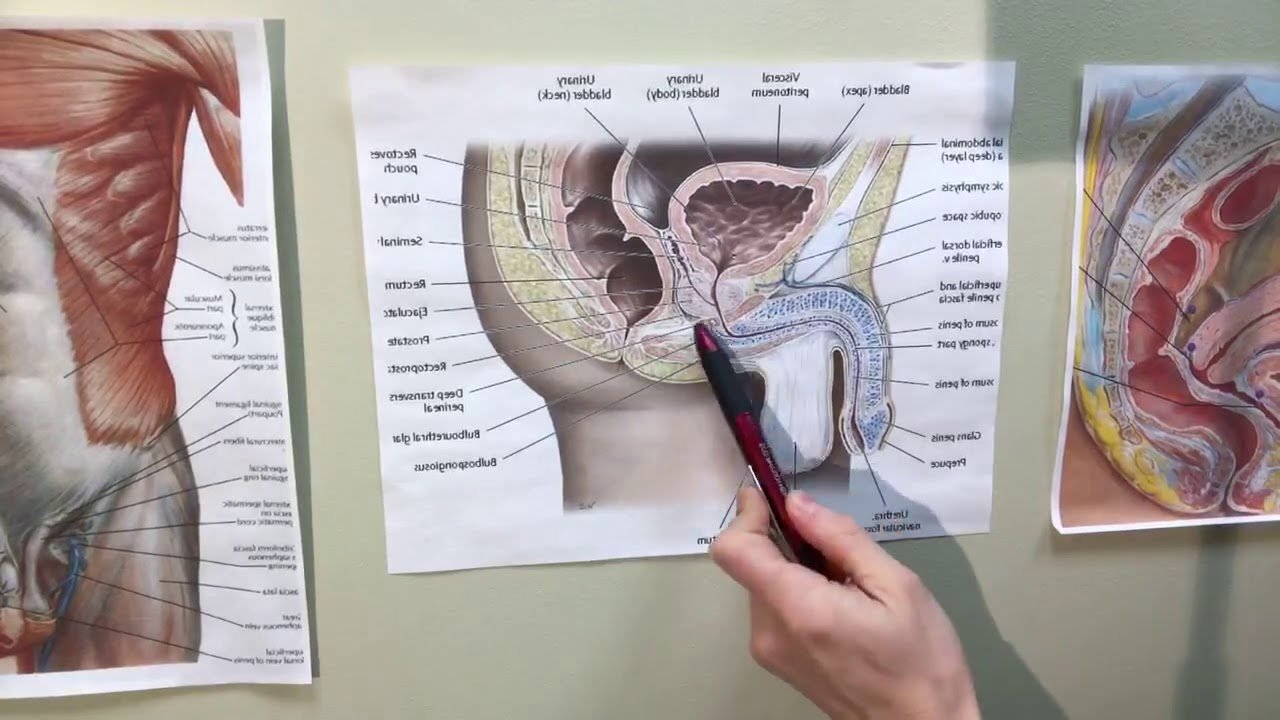
Prostate surgery may be a partial or radical prostatectomy, which is the removal of some or all of the prostate gland, respectively. This is a very delicate operation, and the urethra, bladder, rectum, or urinary sphincter may become damaged in the process.
Because the urethra travels right through the prostate to move urine from the bladder to the penis, the urethra must be cut above and below the prostate in a radical prostatectomy. Once the prostate is removed, the urethra is then reattached directly to the bladder. The man must have a catheter while this area heals.
Moreover, the nerves and muscles in the area may also become damaged. All of this can cause urine to leak, especially when stress is put on the area. You can easily see why stress urinary incontinence is so common after having prostate surgery.
How Is Urinary Incontinence After Prostate Surgery Treated
If you find youre having issues with mild to moderate leakage after surgery, your healthcare provider might suggest starting with noninvasive therapies like medications or physical therapy exercises for the pelvic floor muscles. These treatments may also cut down on the number of times that you have to get up each night to pee.
These methods can sometimes help men who have mild to moderate leakage. Men who have persistent leakage or a more severe problem may need surgery if they do not want to continue to use pads.
Treatment Options For Post
Loss of bladder control after prostate surgery is a devastating complication, which has a significant negative impact on quality of life. The good news is that with appropriate evaluation and treatment, the incontinence problem is usually treatable with significant improvement in quality of life.
It is not unusual that lack of bladder control is a problem for the first few months following radical prostatectomy. A biofeedback program may be helpful during this time period to help restore bladder control. When urinary incontinence persists more than 3-6 months after radical prostatectomy, appropriate bladder testing, called urodynamics, is critical to evaluate the function of the bladder and sphincter muscle to determine the exact cause of the post-prostatectomy incontinence . This urodynamic testing is performed in the office and takes about 20 minutes. The test involves filling the bladder through a special catheter inserted in the penis while measuring the pressures in the bladder. During the test, various maneuvers are performed to evaluate the bladder function, demonstrate the urinary incontinence, and thus specifically define the cause of the urine loss.
Normally, as the bladder fills to capacity, there is very little change in bladder pressure and the sphincter remains closed allowing the man to stay dry. When incontinence occurs following prostatectomy, this normal balance of bladder and sphincter function is disturbed.
Treatment Options:
Male Sling Procedure
Can I Take Medication To Help With My Incontinence
Depending on the degree and length of incontinence you experience, anticholinergics may be recommended to reduce the sensation or frequency of urination.
Decongestants have also been shown to help some patients, though should only be used with physician guidance. An alternative treatment for incontinence uses collagen injections to plump the urinary sphincter for increased urinary control.
The Manual: Products To Help You Deal With Leaking Urine
Urinary incontinence is a common side effect for men after prostate cancer surgery . For some men, lifestyle changes, bladder retraining and pelvic floor muscle exercises will help to reduce or stop the leaking within six to 12 months after surgery. But if not, there are products and treatments available to help. Here Specialist Nurse, Sophie answers some common questions about ways you can manage your incontinence so you can get on with life.
Urine Leakage Long After Prostate Removal
Jun 23, 2020
Leaking urine after prostate surgery is a common problem. Most men report gradual improvement over several months following surgery. However, some men remain incontinent. Certain types of incontinence can be improved with conservative treatment.
There are two main types of incontinence following prostate surgery: urge incontinence and stress incontinence.
I have to go now! Urge incontinence occurs when there is a strong urge to urinate followed by urine leakage. The strong urge to urinate usually indicates an overactive bladder. The prostate is located below the bladder, around the urethra. Some prostate conditions involve slow growth of the prostate resulting in narrowing of the urethra. The bladder must contract strongly to empty through a narrow urethra. This can cause the bladder to become irritable. Unfortunately, in some cases, the bladder remains irritable after the urethra is opened with a prostatectomy.
There are several conservative treatments for urgency. Bladder training involves urinating in the toilet on a timed schedule. Techniques are used to avoid urinating too often. Pelvic floor muscle exercise can also help relax the bladder. Some types of fluid also irritate the bladder and should be eliminated from the diet. A combination of treatments is usually most helpful.
What If These Treatments Do Not Work
If these interventions do not work, you may be referred to a urologist for additional tests on your bladder and sphincter. These tests will determine what type of incontinence you have, how well your bladder is working, and what other treatments might be best for you. This often involves a urodynamic test and a cystoscopy. Both of these procedures are performed in the office, usually during the same visit. They provide your urologist with specific information to help find which procedure might be best for you.
The urodyamics test involves placing a very small catheter in your bladder. This catheter fills the bladder with fluid and measures bladder activity and pressure during filling and voiding . You will also be asked to cough and strain so your provider can see if and how easily you leak urine.
A cystoscopy may also be performed to look at the urethra, the anastomosis , and the bladder. After these tests, your provider will go over the results with you and recommend which treatments are best suited for your condition.
How Can I Help Myself
Urinary problems can affect your self-esteem and independence, and affect your work, social and sex life.
Making some changes to your lifestyle may help, and there are some practical steps that can make things easier.
- Try to drink plenty of fluids, but cut down on fizzy drinks, alcohol, tea and coffee as these may irritate the bladder
- Do regular pelvic floor muscle exercises to help strengthen the muscles that control when you urinate.
- Try to stay a healthy weight. Being overweight can put pressure on your bladder and pelvic floor muscles.
- If you smoke, try to stop. Smoking can cause coughing which puts pressure on your pelvic floor muscles. NHS Choices has more information about stopping smoking
- Plan ahead when you go out. For example, find out where there are public toilets before leaving home.
- Pack a bag with extra pads, underwear and wet wipes. Some men also find it useful to carry a screw-top container in case they cant find a toilet.
- Get our Urgent toilet card to help make it easier to ask for urgent access to a toilet.
- Disability Rights UK runs a National Key Scheme for anyone who needs access to locked public toilets across the UK because of a disability or health condition.
- If you often need to use the toilet at night, leave a light on in case youre in a hurry, or keep a container near your bed.
For more information look at our How to manage urinary problems guide.
A Few Lifestyle Changes
In addition to these innovative solutions, Dr. Cornell may recommend that you also do your part to counteract any urinary incontinence after your prostatectomy. For example, losing weight or voiding your bladder before strenuous activities can help. As well, you should avoid caffeine, which activates your bladder. A few pelvic floor exercises, such as Kegels, can go a long way toward restrengthening the supporting tissues surrounding your bladder and urethra, allowing you better control.
If youre experiencing post-prostatectomy incontinence, please our office in Houston, Texas, to learn more about your treatment options.
You Might Also Enjoy…
Post A Question On Our Forum To Receive Expert Advice
Its rare that men experience long term incontinence after prostate cancer treatment. As a general rule, if your incontinence symptoms last over a year, you should contact a Doctor. There are a number of procedures that exist to restore continence if you do find yourself with long term incontinence.
Practice Good Toilet Habits

Go to the toilet when your bladder feels full dont get into the habit of going just in case. After prostate surgery you may find that you do not experience the sensation of a full bladder. The sensation of a full bladder will gradually return as you are able to hold on longer. It is important to practice holding on to increase the amount of urine your bladder can hold.
Surgical Approaches: Artificial Urinary Sphincter
Surgical intervention for incontinence is typically deferred for at least one year following prostatectomy. Traditionally, the AUS has been the gold standard surgical treatment for SUI after prostatectomy since its introduction several decades ago, offering the advantage of both durability and effectiveness for even severe degrees of incontinence. Initially conceptualized by Foley in 1947, the modern AUS design has evolved over several iterations, with closer resemblance to designs introduced in the 1970s by Scott and Rosen. The present models are fashioned on the concept of using an inflatable fluid-filled cuff surrounding the urethra to control continence in addition to a hydraulic pressure-regulating balloon reservoir and control pump. In the resting activated state, the cuff is inflated, thereby occluding the urethra. When the control pump, implanted in the scrotum, is squeezed manually, the cuff is deactivated. This pumps fluid out of the cuff into the reservoir, thereby depressurizing the cuff and enabling the patient to void. Unless locked in the deactivated state, the cuff automatically reactivates over the subsequent 45 to 90 seconds following deactivation to prevent further flow of urine through the urethra.
Are There New Techniques That Reduce The Chance Of Becoming Incontinent
When removingthe prostate, surgeons try to save as much of the area around the bladder and the sphincter muscles around the urethra as possible, thus limiting damage to the sphincter. Doctors have also fine-tuned the process of placing radioactive seed implants, using sophisticated computer projections that allow the seeds to destroy the prostate while limiting damage to the bladder.
Still, at this point, any man who is undergoing radiation or surgery to treat prostate cancer should expect to develop some problems with urinary control. With newer techniques, some men will have only temporary problems controlling their urine, and many will regain full control of their bladder in time.
Continued
What Is Urinary Incontinence
Urinary incontinence is the involuntary leakage of urine.
In some cases, leakage only occurs in men when they jump, cough, sneeze or laugh. In other cases, leakage can be more severe or continuous, or may occur because they cant get to the toilet in time.
Stress Urinary Incontinence or stress incontinence, is a type of urinary incontinence that happens with physical movement or activity. SUI occurs when control over the external urethral sphincter is damaged or weakened.
Urge incontinence is when you feel the sudden need to urinate but you dont always make it to the toilet in time. It can happen as a result of damage to the bladder or nerves that control the bladder.
Either way, it will be a relief to know that urinary incontinence, no matter how severe, can be treated.
Surgical Approaches: Male Slings
In recent years, various novel surgical treatments have been introduced as alternatives to the AUS. Anti-incontinence procedures can be classified into non-adjustable male slings , adjustable male slings , and adjustable balloon devices . Unlike the AUS, which compresses the urethra circumferentially, thereby interfering with venous blood flow and predisposing the patient to urethral atrophy and even erosion, the male sling compresses only the ventral aspect of the bulbar urethra, leaving the dorsal and lateral blood flow intact. Moreover, tissue, including the bulbospongiosus muscle, is left intact over the urethra, serving as a cushion between the urethra and the sling and further minimizing the risk of erosion.
‘just Cant Wait’ Card
You can get a card to show to staff in shops or pubs etc. It allows you to use their toilets, without them asking awkward questions. You can get the cards from Disability Rights UK or the Bladder and Bowel Community. They also have a map of all the public toilets in the UK.
You could get a key to disabled toilets if you need to access them quickly. You buy the RADAR key from Disability Rights UK. But this should only be used by people who need quick access to a disabled toilet due to a disability or medical condition.
Things To Remember About Male Kegal Exercise
* Make sure you are ONLY using the pelvic muscles. When you are first beginning the male Kegal exercise, you may consider standing in front of a mirror with a hand or on your abdomen or buttocks to feel for movement. It is important that you do NOT use your abdominals, buttocks, or leg muscles. * Remember to breathe normally while exercising. Kegel exercise does not involve holding your breath. * Exercise takes time to strengthen these muscles, just as with any physical therapy. You should start noticing less leakage after 4-6 weeks of consistent daily exercise, and an even larger difference after 3 months. If you do not see an improvement, you may not be exercising the proper muscles. You should be keeping track of how many pads you use per day to monitor your own progress. * Pelvic muscle exercises also improve orgasmic function thereby speeding your return to potency. Contracting these muscles can aid in squeezing more blood into the penis to improve erectile function. * Be pro-active, do your kegel exercises faithfully and you will see results.
Urinary Control Or Continence
Loss of continence is one of the most stress-producing potential side effects of radical prostatectomy because urinary functions are so frequent throughout the day and dysfunction brings into embarrassing highlight what was for most of a mans life an unconscious function requiring little attention.
The Long Wet Road Back To Normal

after radical prostatectomy sucks. But for nearly all men, it goes away. For the very small percentage in whom it doesnt, there is help.
JP Mac is an Emmy award-winning animation writer who worked for Warner Bros. and Disney, and a novelist. He is also very funny.
So, when he wrote a short about his experience with prostate cancer including his diagnosis in 2014 at age 61, the rush to find the right treatment and get it done before his health insurance was going to expire, his laparoscopic-robotic and the complications afterward, and his five-month battle to recover urinary continence after the surgery he could legitimately have written a soap opera, or maybe even a tear-jerker; but he didnt.
Instead, his ebook has a title that sounds like 1950s pulp fiction: They Took My Prostate: Cancer, Loss, Hope. Its not Prostate Cancer Lite, and it doesnt minimize what he or anyone else has gone through to get back to normal after radical prostatectomy. Far from it; in fact, his short, hopeful essay is a testament to what it takes to recover from this difficult but life-saving surgery: a balanced perspective, a good sense of humor, a great support system, and plain old hard work and persistence.
Heres a message you hardly ever hear about prostate cancer, or any illness, for that matter: Its okay to laugh! That doesnt mean its not scary, and that it doesnt wear you down, or that youre not afraid you wont ever get back to normal.
From Three Sphincters to One
Frequent Urination Or Urgency
To help deal with frequent urination and/or the urgent need to urinate it may be helpful to reduce the number of drinks you consume daily that contain alcohol and caffeine. Some beverages and foods can be more likely to irritate your bladder than others, and it may be helpful to try to determine if you have any of these sensitivities. You may find that reducing your intake of the more irritating foods and beverages may help. In addition to alcohol and caffeine, some men find that their bladders are sensitive to carbonated drinks, chocolate, tomatoes, acidic fruits and juices, spicy foods, and artificial sweeteners.
What Causes Incontinence After Prostate Surgery
Urinary incontinence is a potential side effect of prostate removal surgery. The prostate is located just below the bladder and surrounds the urethra. Removing it, or using radiation to treat it, can sometimes cause damage to the nerves and muscles of the bladder, urethra, and or sphincter, which controls the passage of urine from the bladder. This can result in urinary incontinence.
Incontinence After Prostate Surgery: What To Expect
You can rest assured that the incontinence you experience after prostate surgery isnt likely to involve complete bladder emptying. Rather, the short-term incontinence experienced by most is more of a slight drip or leak. This happens most often during strenuous activity or when pressure is placed on the bladder.
There is no standard amount of time that is expected of incontinence. However, patients who experienced normal continence prior to surgery should regain function within 12-13 months of their surgery. There is never an 100% guarantee of this rule, however surgeons work their hardest to cut this time down. Luckily, with the advanced techniques available today, the majority of people should only expect short term side effects.
Does Incontinence Happen If I Treat Prostate Cancer With Radiation
Some men need radiation therapy after prostate removal. During radiation therapy, some of the normal tissues around the urinary sphincter, urethra and bladder may be exposed, causing irritation to occur post therapy, leading to incontinence. This typically subsides within a few months after radiation therapy, however if it persists, additional treatments described below may be helpful.
What You Can Do To Help
Pelvic floor exercises
Pelvic floor exercises target and strengthen the muscles that control your bladder. Your doctor or specialist nurse will talk you through what to do. Research has shown that pelvic floor exercises can help you stop or reduce urine leakage.
If you have not had information about pelvic floor exercises, ask your specialist nurse. Or ask to see a physiotherapist that can talk you through them.
You can find out more about how to do pelvic floor exercises on the NHS website.
Drink plenty of fluids
Dont cut down on your fluids, drink at least 2 litres a day. You can drink plenty during the day, but it might help to limit fluids 2 hours before bedtime. Drinking plenty helps your bladder regain its tone.
Incontinence pads and sheets
You might need to wear pads when you first start going out. There are different types of pads. You might be able to get some pads for free on the NHS, although this may depend on the service in your area. Some GP practices have a continence nurse you can see.
It can also help to visit places where you know there are toilets. Or you can telephone beforehand to find out about toilets and how easy they are to get to.
What Happens After Urethral Sling Surgery
Patients usually recover from this surgery quickly. It’s best to limit demanding activities for approximately six weeks after surgery to avoid having the sling loosen before healing is complete.
After surgery, there may be swelling that makes it difficult to urinate. You’ll have a catheter coming out of the urethra for two to three days. After this, the catheter is removed and just about everyone is able to void on their own. In rare cases, the catheter may have to be reinserted for a few days or up to a week if you cannot urinate.
After the swelling goes down, youll gradually be able to urinate on your own and empty your bladder. However, your normal pattern may not return for a few weeks.
The majority of men who’ve had this procedure have been cured of their urinary incontinence and no longer use pads. The others usually improve to the point where they don’t use as many pads as they were before.
Last reviewed by a Cleveland Clinic medical professional on 10/31/2020.
References
I Often Dont Reach The Toilet When I Need To Go At Night And Sometimes Leak In Bed Is There Anything That Can Help
If you suddenly and urgently need the toilet during the night, you might find hand-held urinals useful. These are containers with a lid that can be used if you cant reach the toilet in time or if there isnt a toilet nearby. You can keep them by your bed and empty it in the morning.
Absorbent pads or pants can stop you wetting the bed if you leak urine in your sleep. You can also get washable or disposable underpads that go on under your sheets, or you could use waterproof bedding to protect your sheets and mattress.
Underpads, waterproof bedding and hand-held urinals are not usually available on the NHS and you cant buy them from supermarkets. But you can order then from chemists or buy them directly from the producers.
Are There New Techniques That Minimize The Chance Of Becoming Incontinent

When removing the prostate, surgeons attempt to conserve as much of the area around the sphincter and the bladder muscles around the urethra as possible, hence curbing damage to the sphincter.
Surgeons have likewise fine-tuned the procedure of putting radioactive seed implants, utilizing advanced computer system forecasts that permit the seeds to damage the prostate while limiting damage to the bladder.
Still, at this point, any male who is going through radiation or surgical treatment to deal with prostate cancer needs to anticipate establishing some issues with urinary control.
Some men will have just temporary issues managing their urine, and lots will gain back complete control of their bladder in time.
Who Is At Higher Risk For These Problems
More invasive procedures carry a higher risk for urinary control issues postoperatively. Many factors can influence urinary control after surgery, including underlying medical conditions, medications, diet, and daily activity. Many of these factors are modifiable, and improvement is often achieved by a comprehensive and motivated approach.
It is important to ask your urologist about urinary control when considering prostate surgery, and to discuss pre-existing urinary control issues. Patient education and motivation are among the most important factors in improving urinary control after prostate surgery.
