Is A Gleason Score Of 9 A Death Sentence
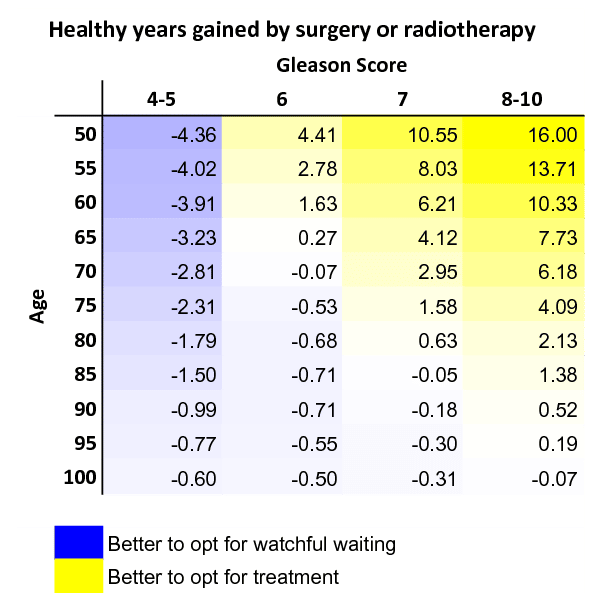
There is a perception among a lot of patients especially when they get diagnosed that having a high Gleason score of 8, 9, or 10 is essentially a death sentence, regardless of how they get treated. This is not actually the case at all. Plenty of men with Gleason 8 to 10 disease actually do well after treatment.
Why Is The Gleason Score Important
According to a study conducted by the University of Geneva, the Gleason score correlates very closely with the clinical behavior of the cancer cells. This makes is a very important indicator of how the cancer will act slowing growing versus aggressive.
It tells oncologists a great deal about the characteristics of the prostate cancer although its not the only tool used to determine whether you need to move ahead with treatment. Other factors are used and evaluated as a whole. This can include one more of the following:
- PSA blood test score
Recommended Reading: How Does A Doctor Test For Prostate Cancer
> > > All Natural Technique Fixes Enlarged Prostate Watch Here< <
Surgical procedures to remove the diseased prostate are usually necessary. Surgical procedures are not always necessary. If the disease is caused by bacterial infections, a doctor can treat the symptoms using alpha-blockers or surgery. Physical therapy, relaxation exercises, and warm baths are all recommended. A physician may also prescribe antibiotics to cure the infection. A bacterial infection can also cause a recurrence of the condition.
An enlarged prostate can be uncomfortable for both men and women. Some of the symptoms of an enlarged male reproductive organ include a weakened urine stream, urgent need to urinate, and urinary tract infections. BPH can also cause damage to the kidneys. A sudden inability to urinate can be life-threatening, as it can lead to bladder and kidney damage. Unfortunately, most men with enlarged prostrates put up with the symptoms for years before they seek treatment. However, many of the men with symptoms finally decide to go to a doctor for proper gynecological evaluation and to begin enlarged prostatic therapy.
You May Like: Is The Prostate An Organ Or A Gland
The Gleason Grading System
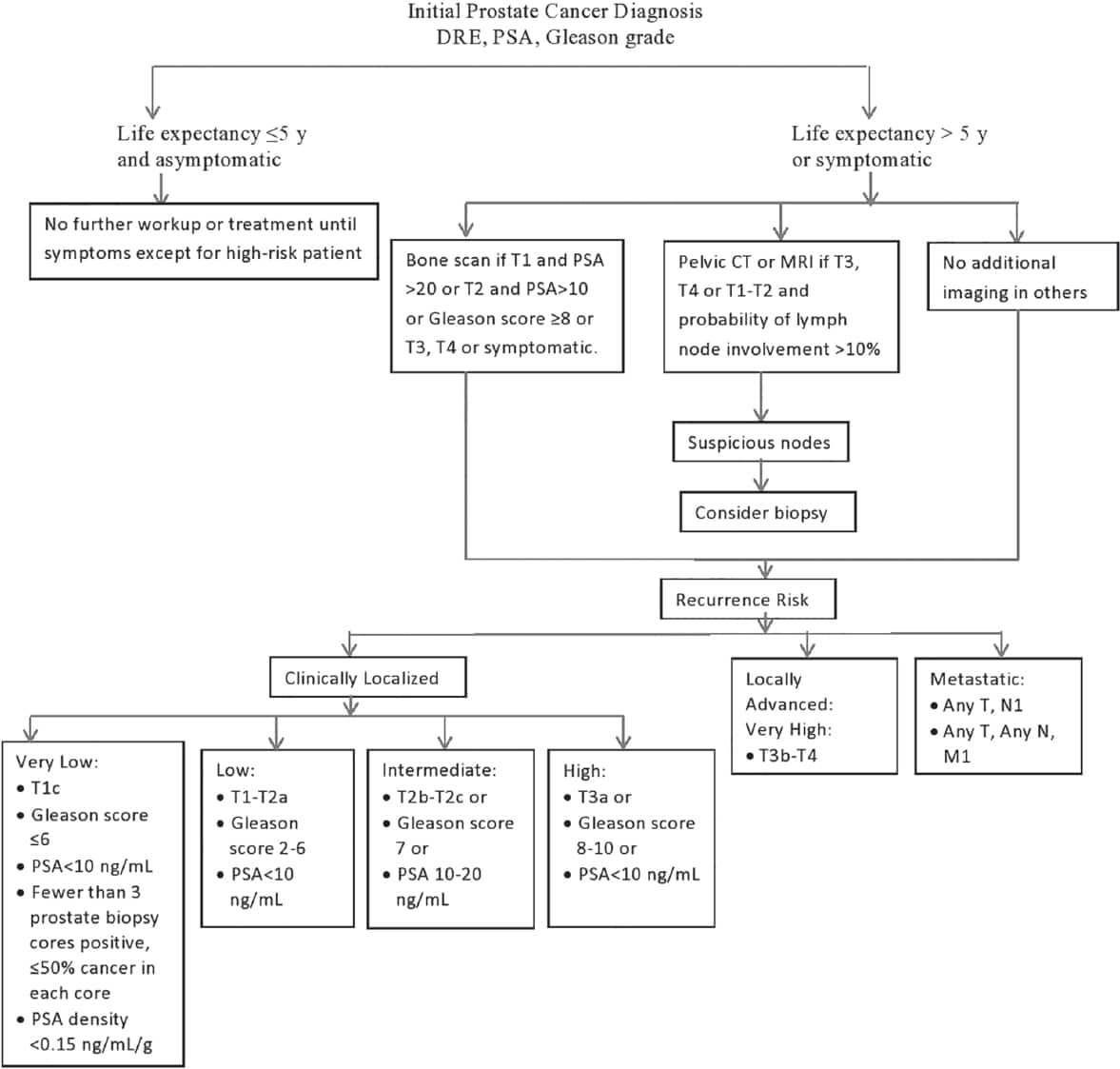
Screening for prostate cancer involves the prostate-specific antigen test and a digital rectal exam. If results are suspect, your doctor may recommend a prostate biopsythe only way to confirm the diagnosis.
During a prostate biopsy, a urologist uses a small needle to remove tissue samples from different parts of the prostate. These samplesalso called coresare then sent to a pathologist so they can review each one under a microscope.
The pathologist uses a pattern scale, developed by Donald Gleason, MD, PhD in 1966, to give each sample a grade from 1 to 5. Grade 1 cells are well-differentiated and look like normal tissue. Grade 5 cells, on the other hand, are “poorly differentiated” or even unrecognizable from normal tissue.
Your Gleason score is the sum of the two numbers that represent the most common types of tissue found in your biopsy. The first number in the equation is the most common grade present, the second number is the second most common grade. For example, if seven of your cores are grade 5 and five are grade 4, your Gleason score would be 5+4, or a Gleason 9.
Today, pathologists typically only flag tissue samples that are grade 3 or higher, making 6 the lowest Gleason score.
In 2014, a revised grading system for prostate cancercalled Grade Groupswas established. This system builds on the Gleason scoring system and breaks prostate cancer into five groups based on risk. This can help make it easier to understand the Gleason score scale.
Movement Builds To Classify Gleason 6 Prostate Lesions As Nonmalignant
In prostate cancer, as in life, you roll the dice.
In craps, 3+3 is called a “hard six.” It’s hard because you can only win if you repeat with a combination of 3+3. Any other sixes you roll — 4+2, 5+1 — are losers.
Gleason 3+3 is a hard six in prostate cancer. It is the lowest grade cancer in the traditional Gleason scoring system. Still, to the eye of a pathologist, a Gleason 6 looks like a malignancy.
Now, a few experts are questioning whether this hard six is a cancer at all. Some urologists see a Gleason 6 as a noncancerous growth that has the potential to be invasive, but most likely will never spread to other organs or end up killing a man.
To a patient like me, who has been on active surveillance for 10 years, a Gleason 6 can create a big medical fuss lasting years with regular prostate-specific antigen blood tests, digital rectal exams , biopsies, and MRIs. It can cause “anxious surveillance” that prompts them to drop AS and undergo unnecessary radical prostatectomy, which poses a potential risk of impotence and urinary incontinence.
The Gleason 6 diagnosis can yield polar opposite recommendations from urologists. Ten years ago, I found this to be the case in the matter of a day.
On December 14, 2010, a local urologist recommended I undergo a radical prostatectomy within the week. When asked, he said he didn’t support active AS, then a relatively new approach for monitoring low-grade prostate cancer.
‘The right thing to do’
Mixed reactions
Recommended Reading: What Color Is Prostate Cancer
Technique Of Focal Therapy
A variety of techniques have been described, all involving the use of directed energy and image guidance. These include high intensity focused ultrasound , MR guided ultrasound, laser ablation, cryosurgical ablation, focal photodynamic therapy, electroporation, various forms of radiation. Ultimately, which of these therapies becomes widely used will be a reflection of precision of treatment, morbidity, cost, and availability and convenience. The principles and methods used with these directed energies have been described previously. The experience with these technologies used for focal therapy is summarized in the table below, in chronological order.
Most of the focal therapy data lacks robust endpoints. In most published studies, follow-up biopsies were usually not systematic, and in most studies the majority of patients were not biopsied. This is a potential source of bias, in that PSA and MRI may misidentify as responders some patients with residual disease. In patients having a biopsy, the rate of positive biopsies ranged from 14% to 50% . Further, most authors only biopsied the treated area. Biopsies of the untreated area were selective based on mpMRI.
What Does It Mean
A Gleason score of 6 is low grade, 7 is intermediate grade, and a score of 8 to 10 is high grade cancer.
Get More Information
Its also important to know whether any cells rated at Gleason grade 5 are present, even in just a small amount, and most pathologists will report this. Having any Gleason grade 5 in your biopsy or prostate puts you at a higher risk of recurrence.
But because many prostate cancer cases are extremely slow-growing, the Gleason system didnt necessarily do a good job of communicating the risks for these cases. Patients with scores of 6 and 7 didnt have a clear picture of the nature of their particular cancer.
Recommended Reading: What Is The Purpose Of Your Prostate
Challenges To Conventional Wisdom In Prostate Cancer
Bert Vorstman, MD, MS
Patients with prostate cancer have a right to expect that their screening, diagnosis, and treatment are supported by evidence-based science. But how well does the urology community measure up when it comes to claims that standard-of-care practices are evidence based?
Fifteen years ago, meta-researcher John Ioannidis, PhD, published a seminal essay since viewed more than 3.2 million times arguing “most published research findings are false.” Ioannidis’s concerns are especially pertinent for clinicians who assume that their testing and treatment philosophies are inherently valid on the basis of studies designed to support these unfounded biases.
Here are five evidence-based challenges to conventional dogma in prostate cancer treatment.
1. The rapid growth of prostate cancer treatment is not driving increased survival.
The North American market for prostate cancer treatments is poised to reach USD $30.6 billion by 2025. Yet, the annual US death rate is about 30,000 and slowly decreasing as each decade passes. Surprisingly, this improvement in mortality is probably not based on early detection and treatment but rather on the effect of a gradual increase in life expectancy due to better treatment of infections and comorbidities.
2. Gleason score 6 is not prostate cancer.
3. PSA-based screening does not save lives.
4. Prostate cancer surgery for localized prostate cancer does not improve survival.
A Gleason 6 Tumor: Is It Cancer And Should It Be Treated
The issue is not what we call a Gleason 6, but whether it has the potential to progress. Researchers currently are looking at genetic signatures that can differentiate a nonthreatening Gleason 6 from one that will progress to Gleason 7 or higher and possibly metastasize. Richard J. Ablin, PhD, DSc Tweet this quote
The diagnosis and treatment of prostate cancer have long been a source of controversy among the oncology community, the political sector, and patient advocacy groups. Most notably, the decision to biopsy a mans prostate gland rests largely on his prostate-specific antigen test numbers, the accuracy and clinical value of which have been hotly debated for decades, and still no consensus has been reached. A new controversial question has arisen in prostate cancer: Is a tumor with a Gleason 6 score a potential killer, or should it be left alone? About 180,000 American men are diagnosed with prostate cancer each year, and their clinicians need guidance on this critical question.
Is a Gleason 6 Tumor Cancer?
Herbert Lepor, MD
Dr. Lepor continued: What is unknown is whether Gleason 6 cancers on the basis of genetic instability can evolve into a higher Gleason tumor and then metastasize. So if we knew that a prostate harbored only Gleason 6 disease and over time the disease would not de-differentiate, then Gleason 6 disease would not metastasize and by definition would not be a cancer. Unfortunately, this is not so simple.
Better Selection Needed
Sharp Disagreement
Don’t Miss: Are Walnuts Good For Your Prostate
The Gleason 6 Cancer Deception
The all-inclusive prostate cancer label is deceitful by implying that all prostate cancers are equal and have the power to kill rapidly whereas it has been well established that the very common Gleason 6 type of prostate cancer fails to behave as a cancer and, should not be called a cancer.
In fact, Larry Klotz M.D. and others, have shown irrefutably that the Gleason 6 prostate cancer is a not a real cancer at all for two fundamental reasons: no man has died from this disease and, this so-called cancer lacks a number of molecular biological mechanisms normally found in cancerous behaving cells. Furthermore, unlike a typical cancer cell, this cell has a very long doubling time at 475 +/ 56 days so that from mutation to a growth of about 1 cm in diameter takes some 40 years.
Therefore, because the Gleason 6 lacks the hallmarks of a cancer, it is not a health risk, it does not progress to become a health risk, needs no detection and, needs no treatment. The Gleason 6 is a pseudo-cancer mislabeled as a cancer this false cancer tag is a monstrous medical error and public health disaster, inviting legal retribution. Only the 15% or so of the high-grade forms of prostate cancers have the potential to kill and, only they demand detection and treatment.
What Does It Mean If My Biopsy Report Mentions The Word Core
The most common type of prostate biopsy is a core needle biopsy. For this procedure, the doctor inserts a thin, hollow needle into the prostate gland. When the needle is pulled out it removes a small cylinder of prostate tissue called a core. This is often repeated several times to sample different areas of the prostate.
Your pathology report will list each core separately by a number assigned to it by the pathologist, with each core having its own diagnosis. If cancer or some other problem is found, it is often not in every core, so you need to look at the diagnoses for all of the cores to know what is going on with you.
Read Also: How Much Does A Normal Prostate Weigh
Diagnostic Tests Are Limited
We always knew that prostate cancer is common and that, until recently, it often went undiagnosed: Autopsies of men who died of other causes have shown that about one-third of men over age 50 have some cancerous cells in their prostate, while 90% of men over age 90 have such cells.
As PSA screening has grown more widespread, we are finding more tumors that otherwise would have escaped detection. Yet current diagnostic technology does not always enable urologists to determine which tumors will lie dormant and which will become active, spreading elsewhere in the body.
Studies estimate that anywhere from 16%56% of men diagnosed with prostate cancer, generally because of an abnormal PSA test, have tumors that might never have caused problems had they not been found. And the landmark Prostate Cancer Prevention Trial unexpectedly yielded data that early-stage prostate tumors are incredibly common, even at PSA levels considered normal.
The PCPT was a randomized controlled study the type considered to be the gold standard in research . The study, which involved almost 19,000 healthy men, was designed to evaluate whether the drug finasteride could prevent prostate cancer from developing. Finasteride is a hormonal medication originally approved to treat benign prostatic hyperplasia , but which has also been investigated as a potential treatment for prostate cancer.
Exceptions And Barriers To Active Surveillance
In his UCSF program, Dr. Cooperberg said, about 95% of men diagnosed with low-risk prostate cancer are put on active surveillance. As an academic center that began implementing and studying active surveillance in the mid-1990s, thats likely higher than what is typically seen in the United States, he acknowledged.
But a reasonable target for the time being is around 80%, he said. Thats consistent with where rates top out in countries like Sweden and in other large, integrated health care systems in Europe where active surveillance has long been standard practice.
The bottom line, Dr. Cooperberg said, is that even though the vast majority of men with low-risk prostate cancer should be put on active surveillance, there will always be exceptions.
Those exceptions, for example, can include men with a strong family history of prostate cancer or who have urological symptoms related to the disease that immediate treatment can help to alleviate.
There can also be considerations that go beyond clinical or biological factors. For patients in rural areas or those who lack reliable transportation, anything that requires regular visits to the hospital or doctors office over a long period could push some men toward choosing immediate treatment, Dr. Watts said.
In addition, she noted, it can be challenging to explain the medical basis for active surveillance. In some patients minds, opting for active surveillance means missing a window of opportunity for cure, she said.
You May Like: Is Cialis Good For Enlarged Prostate
What Does It Mean If In Addition To Cancer My Biopsy Report Also Mentions Acute Inflammation Or Chronic Inflammation
Inflammation of the prostate is called prostatitis. Most cases of prostatitis reported on biopsy are not caused by infection and do not need to be treated. In some cases, inflammation may increase your PSA level, but it is not linked to prostate cancer. The finding of prostatitis on a biopsy of someone with prostate cancer does not affect their prognosis or the way the cancer is treated.
Gleason 6 Prostate Cancer: Serious Malignancy Or Toothless Lion
Nicholas M. Donin, MDOncology
There is strong evidence from longitudinal cohort studies of men with both treated and untreated Gleason 6 prostate cancer to suggest that Gleason 6 disease, when not associated with higher-grade cancer, virtually never demonstrates the ability to metastasize and thus represents an indolent entity that does not require treatment.
Autopsy studies of men without known prostate cancer suggest that a substantial reservoir of prostate cancer that does not cause symptoms or death exists within the population. The majority of these cancers are Gleason 6 tumors and are frequently detected by prostate-specific antigenbased prostate cancer screening. There is strong evidence from longitudinal cohort studies of men with both treated and untreated Gleason 6 prostate cancer to suggest that Gleason 6 disease, when not associated with higher-grade cancer, virtually never demonstrates the ability to metastasize and thus represents an indolent entity that does not require treatment. Whether Gleason 6 has a propensity to progress to higher-grade cancer is still under investigation. Because the term cancer has historically been used to represent a disease state that leads to progressive illness that is uniformly fatal without treatment, we believe Gleason 6 disease should not be labeled with this term. Our challenge now is to develop the technology to differentiate true Gleason 6 disease from the higher grades of dysplasia with which it can be associated.
Read Also: How To Stimulate Your Prostate
Epidemiologic Support For The Concept Of Clinically Insignificant Prostate Cancer
All available evidence suggests that there is a substantial reservoir of prostate cancer within the population that does not result in clinical symptoms or death. The best evidence for the existence of such a reservoir comes from studies examining prostates obtained from autopsies, as well as studies of specimens obtained during cystoprostatectomy performed for aggressive bladder cancer in which the prostate is removed incidentally. Autopsy studies from multiple countries have demonstrated a prevalence of undiagnosed prostate cancer in the population that ranges from approximately 18% to 40%. Of these incidentally detected cancers, at least 80% were exclusively Gleason pattern 3 disease. Specimens from cystoprostatectomy performed for bladder cancer exhibit a somewhat higher rate of malignancy overall, ranging between 41% and 54%, but the prevalence of high-grade elements is also quite low, with > 70% demonstrating only Gleason pattern 3.
Taken together, these studies reveal the presence of a large reservoir of prostate cancers, the majority of which are Gleason 6, which exist in the population and do not cause clinical symptoms or death. Many of these prostate cancers could potentially be diagnosed by PSA screening and random systematic biopsy, suggesting that a substantial proportion of Gleason 6 disease detected by PSA screening represents disease that may never lead to metastasis or death.
