Multiparametric Magnetic Resonance Imaging
The National Comprehensive Cancer Network advises that although standard MRI techniques can be considered for initial evaluation of high-risk patients, multiparametric magnetic resonance imaging can be used in the staging and characterization of prostate cancer. mpMRI images are defined as those acquired with at least one more sequence in addition to the anatomic T2-weighted images, such as diffusion-weighted imaging and dynamic contrast images. In addition, the NCCN guidelines recommend considering mpMRI in patients undergoing active surveillance if anterior and/or aggressive cancer is suspected when PSA increases and systematic prostate biopsies are negative.
The 2016 EAU/ESTR/SIOG guidelines recommend mpMRI prior to performing a repeat biopsy when clinical suspicion of prostate cancer persists in spite of negative biopsies. During repeat biopsy, target any mpMRI lesions seen. Additionally, the guidelines recommend performing mpMRI for local staging and metastatic screening in predominantly Gleason pattern 4 intermediate risk patients and for local staging in high-risk localised prostate cancer.
Guidelines For Recommending A Bone Scan
We examined the European Association of Urology guidelines,3 American Urological Association PSA best practice policy,1 the guidelines of the National Comprehensive Cancer Network ,4 and the classification and regression tree by Briganti and colleagues.2
According to the EAU guidelines, a bone scan may not be indicated in asymptomatic patients with a well or moderately differentiated tumour if the serum PSA level is < 20 ng/mL. Based on the AUA guidelines, a bone scan is unnecessary with localized disease when the serum PSA level is < 20 ng/mL and there is no clinical evidence of bone metastasis. A bone scan is appropriate according to the NCCN guidelines for symptomatic patients and/or those with life expectancy > 5 years when they have any of the following: T1 disease with PSA > 20 ng/mL or T2 disease with PSA > 10 ng/mL, GS 8, or T3 or T4 or symptomatic disease. According to Brigantis CART, a bone scan should be considered only for patients with a GS > 7 or serum PSA level > 10 ng/mL with a palpable tumour .
> > > 1 Bedtime Hack To Pee Like A Bull
An enlarged prostate can also be the cause of other problems. If the enlarged prostate is causing symptoms, the best treatment would be a natural remedy. In the meantime, there are treatments for a wide range of conditions that cause a man to experience pain. A common surgical procedure involves an electric loop, laser, or electro-stimulation. The procedure is a safe and effective option for treating enlarged or symptomatic BPH.
Recommended Reading: Can You Survive Prostate Cancer
Comparison Among Guideline Results
The EAU and AUA guidelines showed 100% agreement in recommending a bone scan. However, the McNemar test showed that the bone scan recommendations differed significantly in other comparisons .
Pairwise comparisons of the ROC curves showed that the AUA and EAU guidelines had larger areas under the curve than did the other guidelines . No significant difference was detected between the AUA and EAU guidelines. Among the 806 patients, 16 had bone metastasis even though none of guidelines recommended a bone scan.
Receiver operating characteristic curve analyses . Note: Pairwise comparison of ROC curves shows significant result with p < 0.05 in AUA vs. Brigantis CART, AUA vs. NCCN, Brigantis CART vs. EAU, Brigantis CART vs. percent positive core, EAU vs. NCCN, NCCN vs. percent positive core. AUA: American Urological Association EAU: European Association of Urology NCCN: National Comprehensive Cancer Network Brigantis CART: Brigantis classification and regression tree.
About Dr Dan Sperling
Dan Sperling, MD, DABR, is a board certified radiologist who is globally recognized as a leader in multiparametric MRI for the detection and diagnosis of a range of disease conditions. As Medical Director of the Sperling Prostate Center, Sperling Medical Group and Sperling Neurosurgery Associates, he and his team are on the leading edge of significant change in medical practice. He is the co-author of the new patient book Redefining Prostate Cancer, and is a contributing author on over 25 published studies. For more information, contact the Sperling Prostate Center.
Search the spc blog
Also Check: What Does Elevated Prostate Levels Mean
Don’t Miss: Does Masturbation Help The Prostate
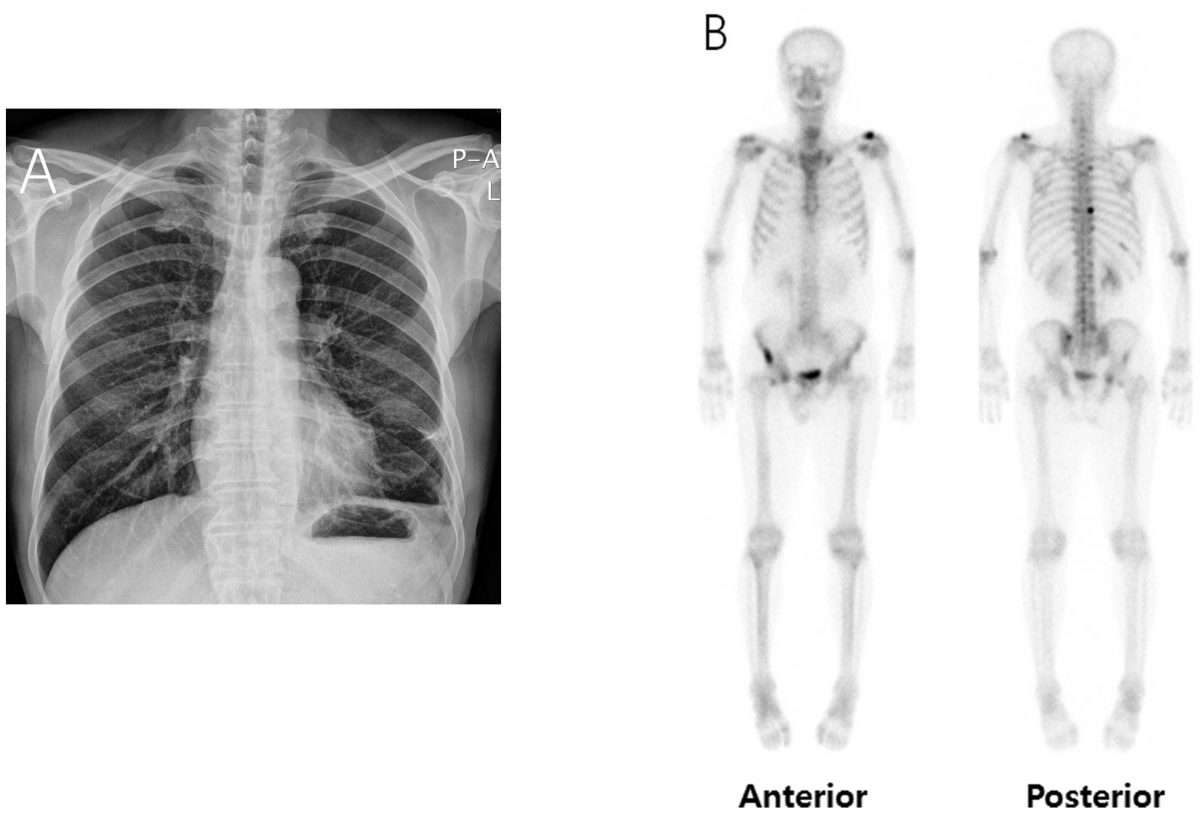
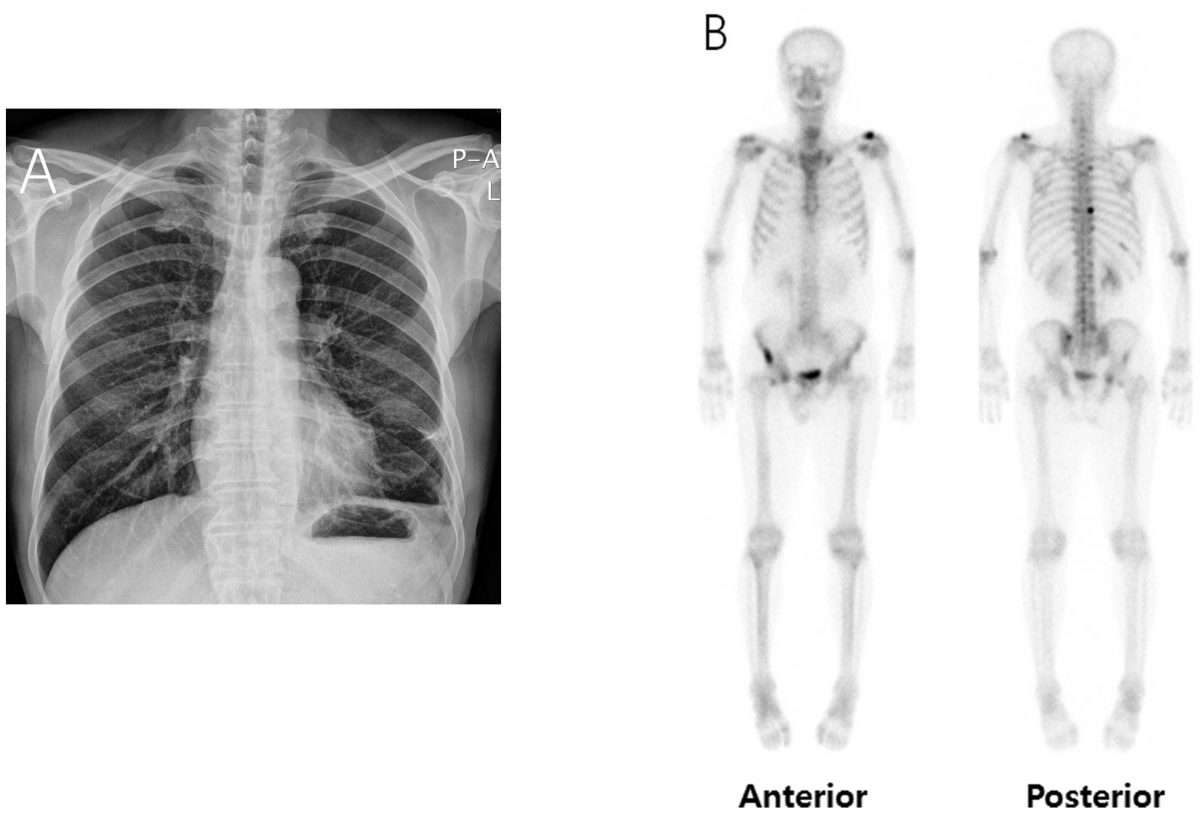
Bone Scan For Diagnosis Of Metastatic Disease
Current NCCN guidelines include scanning technology utilizing fluorine-18 sodium fluoride as the tracer for the subsequent positron-emission tomography scan as an option for men with prostate cancer who undergo a bone scan to search for metastatic disease. PET and hybrid imaging bone scans appear more sensitive than conventional 99-technetium bone scans.
Rising Psa After Radiotherapy And Negative Conventional Imaging
For men for whom salvage local or regional therapy is not planned or is inappropriate, there is little evidence that NGI will alter treatment or prognosis. The role of NGI in this scenario is unclear and it should not be offered, except in the context of an institutional review boardapproved clinical trial.
For men for whom salvage local or regional therapy is contemplated, evidence supports NGI for detection of local and/or distant sites of disease. Findings on NGI could guide management in this setting . PSMA imaging , 11C-choline or 18F-fluciclovine PET/CT or PET/MRI, whole-body MRI, and/or 18F-NaF PET/CT can provide superior disease detection compared with conventional imaging and their results may alter patient management, although data are limited.
Also Check: What Are The Stages Of Prostate Cancer
Imaging Tests For Prostate Cancer
Imaging tests use x-rays, magnetic fields, sound waves, or radioactive substances to create pictures of the inside of your body. One or more imaging tests might be used:
- To look for cancer in the prostate
- To help the doctor see the prostate during certain procedures
- To look for spread of prostate cancer to other parts of the body
Which tests you might need will depend on the situation. For example, a prostate biopsy is typically done with transrectal ultrasound and/or MRI to help guide the biopsy. If you are found to have prostate cancer, you might need imaging tests of other parts of your body to look for possible cancer spread.
The imaging tests used most often to look for prostate cancer spread include:
European Association Of Urology/european Society For Radiotherapy And Oncology/international Society Of Geriatric Oncology Recommendations
EAU, ESTRO and SIOG released a joint clinical practice guideline for prostate cancer in 2016. The guideline recommendations for patients with mCRPC include the following :
-
Treat with life prolonging agents . Base the choice of first line treatment on the performance status, symptoms, comorbidities and extent of disease.
-
Candidates for cytotoxic therapy should be offered docetaxel with 75 mg/m2 every 3 weeks.
-
In patients with progression following docetaxel chemotherapy, offer further life-prolonging treatment options, which include cabazitaxel, abiraterone, enzalutamide and radium-223.
-
Offer bone protective agents to patients with skeletal metastases to prevent osseous complications. However, the benefits must be balanced against the toxicity of these agents, and jaw necrosis, in particular, must be avoided.
-
Offer calcium and vitamin D supplementation when prescribing either denosumab or bisphosphonates.
-
Treat painful bone metastases early on with palliative measures such as EBRT, radionuclides, and adequate use of analgesics.
-
In patients with spinal cord compression, start immediate high-dose corticosteroids and assess for spinal surgery followed by irradiation. Offer radiation therapy alone if surgery is not appropriate.
Recommended Reading: Can Enlarged Prostate Cause Blood In Urine
Medical History And Physical Exam
If your doctor suspects you might have prostate cancer, he or she will ask you about any symptoms you are having, such as any urinary or sexual problems, and how long you have had them. You might also be asked about possible risk factors, including your family history.
Your doctor will also examine you. This might include a digital rectal exam , during which the doctor inserts a gloved, lubricated finger into your rectum to feel for any bumps or hard areas on the prostate that might be cancer. If you do have cancer, the DRE can sometimes help tell if its only on one side of the prostate, if its on both sides, or if its likely to have spread beyond the prostate to nearby tissues. Your doctor may also examine other areas of your body.
After the exam, your doctor might then order some tests.
Preparing For Your Bone Scan
You can eat and drink normally before your scan. Take your medicines as normal unless your doctor tells you otherwise.
Phone the department where you are having the scan if you are pregnant or breastfeeding. You might have to stop breastfeeding for a short period of time after having the scan. So you might want to store enough expressed milk for 1 or 2 feeds beforehand. The staff at the department will advise you.
You have to arrive at the hospital about 4 hours before your scan. Your appointment letter will tell you the exact time.
Tell the department beforehand if you have difficulties passing urine, need to pass urine urgently, or have prostate related problems.
Don’t Miss: What Are The Five Stages Of Prostate Cancer
Developing Landscape For Non
Non-metastatic CRPC prevalence has been estimated at 7% of PCa in the European Union . Owing to the advent of modern imaging, the prevalence of this subgroup has declined. These newer imaging agents i.e., fluciclovine or PSMA can identify local recurrence or metastases at PSA levels far below the traditional PSA threshold for other imaging modalities such as CT or bone scan. Some of the new PET agents can identify metastatic lesions at PSA values as low as 0.20.5 ng/mL, allowing the prompt identification of M1 CPRC . This is interesting given the recent randomized studies in this field , which show the efficacity of apalutamide and enzalutamide . The metastasis-free survival of patients with nmCRPC was previously estimated as ~2530 months, but can now be significantly prolonged using combination next-generation hormone therapy with ADT . The use of PSA doubling time to determine risk for progression can guide the appropriate timing for starting therapy. For instance, a PSA doubling time 10 months is appropriate to initiate therapy. There is no currently established standard of care option for treatment of this population, hence the need for enrollment in clinical trials .
Identifying Models Used For Selective Bone Scan Staging
Models were chosen from published literature and guidelines and validated in the South Australian Prostate Cancer Clinical Outcomes Collaborative database. A model was defined as any allocation of bone scan positivity risk to a group of newly diagnosed prostate cancer patients based on a predictor. MEDLINE and EMBASE databases were searched for models using keywords: Prostate Cancer, Metastases, Prediction, Staging, Screening and Imaging and an English-only limit. Titles and abstracts were screened for relevance. Abstract-only records and reviews were manually excluded. Articles containing models predicting bone scan positivity, using common clinical predictors, were further assessed. Those using tests not routinely available were excluded. Common predictors included serum Prostate Specific Antigen, Tumour stage and Gleason score at diagnosis. We used the Prediction model Risk Of Bias ASsessment Tool tool for quality assessment.
Read Also: Is Drinking Coffee Bad For Your Prostate
Use In Men Who Might Have Prostate Cancer
The PSA blood test is used mainly to screen for prostate cancer in men without symptoms. Its also one of the first tests done in men who have symptoms that might be caused by prostate cancer.
PSA in the blood is measured in units called nanograms per milliliter . The chance of having prostate cancer goes up as the PSA level goes up, but there is no set cutoff point that can tell for sure if a man does or doesnt have prostate cancer. Many doctors use a PSA cutoff point of 4 ng/mL or higher when deciding if a man might need further testing, while others might recommend it starting at a lower level, such as 2.5 or 3.
- Most men without prostate cancer have PSA levels under 4 ng/mL of blood. Still, a level below 4 is not a guarantee that a man doesnt have cancer.
- Men with a PSA level between 4 and 10 have about a 1 in 4 chance of having prostate cancer.
- If the PSA is more than 10, the chance of having prostate cancer is over 50%.
If your PSA level is high, you might need further tests to look for prostate cancer.
To learn more about how the PSA test is used to look for cancer, including factors that can affect PSA levels, special types of PSA tests, and what the next steps might be if you have an abnormal PSA level, see Screening Tests for Prostate Cancer.
Read Also: Show Me A Picture Of A Mans Prostate
Getting The Results Of The Biopsy
Your biopsy samples will be sent to a lab, where they will be looked at with a microscope to see if they contain cancer cells. Getting the results usually takes at least 1 to 3 days, but it can sometimes take longer. The results might be reported as:
- Positive for cancer: Cancer cells were seen in the biopsy samples.
- Negative for cancer: No cancer cells were seen in the biopsy samples.
- Suspicious: Something abnormal was seen, but it might not be cancer.
If the biopsy is negative
If the prostate biopsy results are negative , and the chance that you have prostate cancer isnt very high based on your PSA level and other tests, you might not need any more tests, other than repeat PSA tests sometime later.
But even if many samples are taken, biopsies can still sometimes miss a cancer if none of the biopsy needles pass through it. This is known as a false-negative result. If your doctor still strongly suspects you have prostate cancer , your doctor might suggest:
- Getting other lab tests to help get a better idea of whether or not you might have prostate cancer. Examples of such tests include the Prostate Health Index , 4Kscore test, PCA3 tests , and ConfirmMDx. These tests are discussed in Whats New in Prostate Cancer Research?
- Getting a repeat prostate biopsy. This might include getting additional samples of parts of the prostate not biopsied the first time, or using imaging tests such as MRI to look more closely for abnormal areas to target.
Prostate cancer grade
Also Check: How Do You Massage The Prostate
American Urological Association Recommendations
American Urological Association guidelines for the management of CRPC describe six index-patient scenarios for which recommendations could be formulated.
Index patient no. 1: Asymptomatic non-metastatic CRPC
Recommendations are as follows:
-
Observation with continued ADT
-
First-generation antiandrogens or first-generation androgen-synthesis inhibitors to patients unwilling to accept observation.
-
Systemic chemotherapy or immunotherapy should not be offered to patients with non-metastatic CRPC outside the context of a clinical trial
Index patient no. 2: Asymptomatic or minimally-symptomatic, metastatic CRPC with good performance status and without prior docetaxel chemotherapy
Recommendations are as follows:
-
Abiraterone plus prednisone, enzalutamide, docetaxel, or sipuleucel-T
-
First-generation antiandrogen therapy or ketoconazole plus steroid or observation to patients who do not want or cannot have one of the standard therapies
Index patient no. 3: Symptomatic, metastatic CRPC with good performance status and no prior docetaxel chemotherapy
Recommendations are as follows:
-
Docetaxel
-
Abiraterone plus prednisone, enzalutamide, or docetaxel
-
Ketoconazole plus steroid, mitoxantrone, or radionuclide therapy for patients who do not want or cannot have one of the standard therapies
-
Radium-223 to patients with symptoms from bony metastases and without known visceral disease
-
Treatment with either estramustine or sipuleucel-T should not be offered
Recommendations are as follows:
Bone Scan And Imaging Studies
The Current Procedural Technology/Healthcare Common Procedure Coding System codes in Medicare data provided information regarding imaging, procedures, and treatments. Bone scans performed after date of diagnosis and before the earlier of 180 days or date of first treatment were considered part of the initial staging workup. Because SEER provides only the month and year of diagnosis, we assigned each patients diagnosis to the first of each month and deemed this reasonable because bone scans are unlikely to be used for purposes other than cancer staging.
For patients who received a bone scan, we then examined uses of additional imaging and procedures: x-ray, CT, and MRI specific to bone evaluation, and bone biopsy. We defined imaging and procedures performed within 90 days after bone scan and before treatment as potential downstream studies to further work-up abnormalities identified on bone scan. A complete list of HCPCS codes is shown in the .
Recommended Reading: Gleason Level 6 Prostate Cancer
Don’t Miss: What Does The Prostate Produce
Newly Diagnosed Clinically High
When conventional imaging is negative in patients with a high risk of metastatic disease, NGI may add clinical benefit, although prospective data are limited.
When conventional imaging is suspicious or equivocal, NGI may be offered to patients for clarification of equivocal findings or detection of additional sites of disease, which could potentially alter management, although prospective data are limited.
Early Versus Delayed Treatment
In the years following the introduction by Huggins and Hodges of hormone therapy for prostate cancer, early institution of such treatment was recommended based on comparison with historical controls.
Later, the Veterans Administration Cooperative Urology Research Group studies reversed the recommendation of early hormone therapy instead, hormone therapy was deferred until symptomatic progression. In addition, prolongation of survival was believed to be secondary to the alteration of the nature of metastatic lesions, thereby creating earlier androgen resistance, rather than a result of early hormone manipulation.
In more recent years, the old controversy of appropriate androgen-deprivation therapy timing has gained new and stronger popularity because of the advent of less-toxic and well-tolerated pharmaceutical agents, such as luteinizing hormone-releasing hormone agonists and antiandrogens. Laboratory studies have demonstrated that early hormone therapy does not confer early resistance. An update of the VACURG study by Byar and Corle determined that disease progression from stage C to stage D was decreased from 50% to 10% with diethylstilbestrol therapy. Crawford and associates also showed a benefit of early hormone therapy in patients with distant metastases.
Also Check: When Should Guys Get A Prostate Exam
